What is an anxiety disorder?
Everybody experiences situations where they are anxious or afraid, such as right before an exam or job interview. Feeling anxious or afraid at times is normal and even healthy. If, however, the anxiety levels are too high and keep you from your daily activities, work or social obligations, then it is possible that you are suffering from one of the anxiety disorders.
Anxiety disorders are mental disorders characterized by significant feelings of anxiety and fear. It is important to note that anxiety refers to worrying about future events, whereas fear refers to a reaction on current events [1]. Both anxiety and fear may cause physical and emotional symptoms, such as sweating, racing hart, fright, and panic, but can also cause people to worry a lot, to avoid places and situations, and sometimes even to keep people at home.
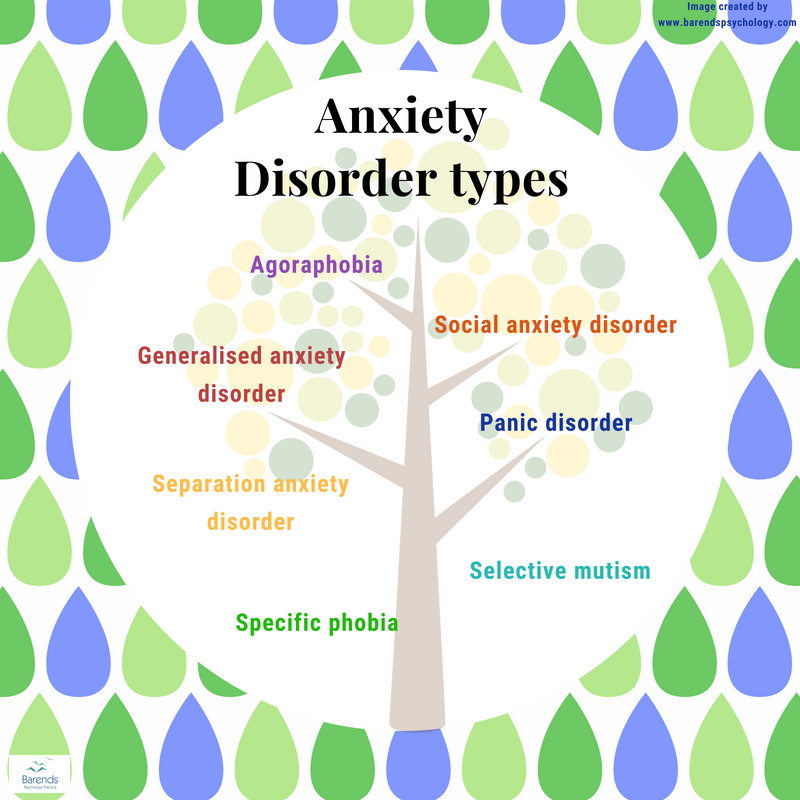
There are several anxiety disorders: social anxiety disorder, generalized anxiety disorder, specific phobia, panic disorder, Agoraphobia, separation anxiety disorder, and selective mutism. Each anxiety disorder has its own set of symptoms, age of onset, treatment, and impact on daily life. This page briefly discusses their differences.
Go to:
At Barends Psychology Practice, treatment for anxiety disorders is being offered. Contact us to schedule a first, free of charge, first session. (Depending on your health insurance, treatment may be reimbursed).
Anxiety disorders – Social anxiety disorder
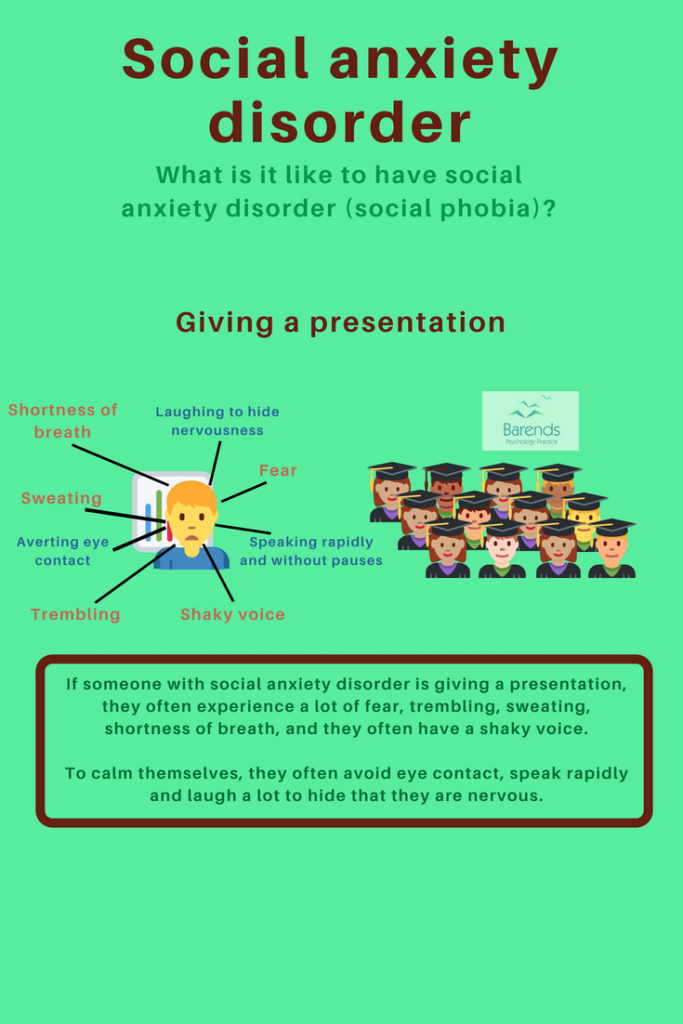
Social anxiety disorder (or social phobia) is characterized by an excessive and unreasonable fear of social situations. People with social anxiety disorder (SAD) usually experience a lot of stress, anxiety, and fear if they have to speak in public, talk in a (small) group of people or perform something in front of an audience. The feeling of being watched, criticized or judged by others causes them to be very self-conscious and nervous, because they are afraid of making mistakes, embarrass or humiliate themselves. It is common for someone with SAD to avoid social situations if there is a fair chance of them becoming the center of attention.
Age of onset is between 12 and 16.6 years [2],[3],[4],[7]. Depending on the populations used for the studies, between 7.4 and 13 out of 100 persons have social anxiety disorder at one point in their lifetime [5],[6],[7],[9].
Safety behaviour: it is common for people with SAD to use safety behaviour or safety signals to help them calm down. Examples are: taking a friend to a party, having a few alcoholic beverages at the start of an event, taking deodorant or a certain necklace with you.
Symptoms:
- Anxiety or fear in social situations, in which a person feels scrutinized, noticed or observed.
- Fear of showing their anxiety or fear and being socially rejected.
- Social interactions are avoided or reluctantly endured.
- Social interactions provokes constant stress.
- Social anxiety causes personal distress and impairs someone on certain domains such as occupational or social.
- Fear and anxiety are out of proportion to the situation.
- The above mentioned symptoms are present for more than 6 months.
For more information about Social Anxiety Disorder, please go to:
- Social anxiety disorder treatment.
- Social anxiety test.
- Coping with social anxiety.
- Partner has social anxiety. (coming soon)
- Social anxiety facts.
Anxiety disorders – Panic disorder
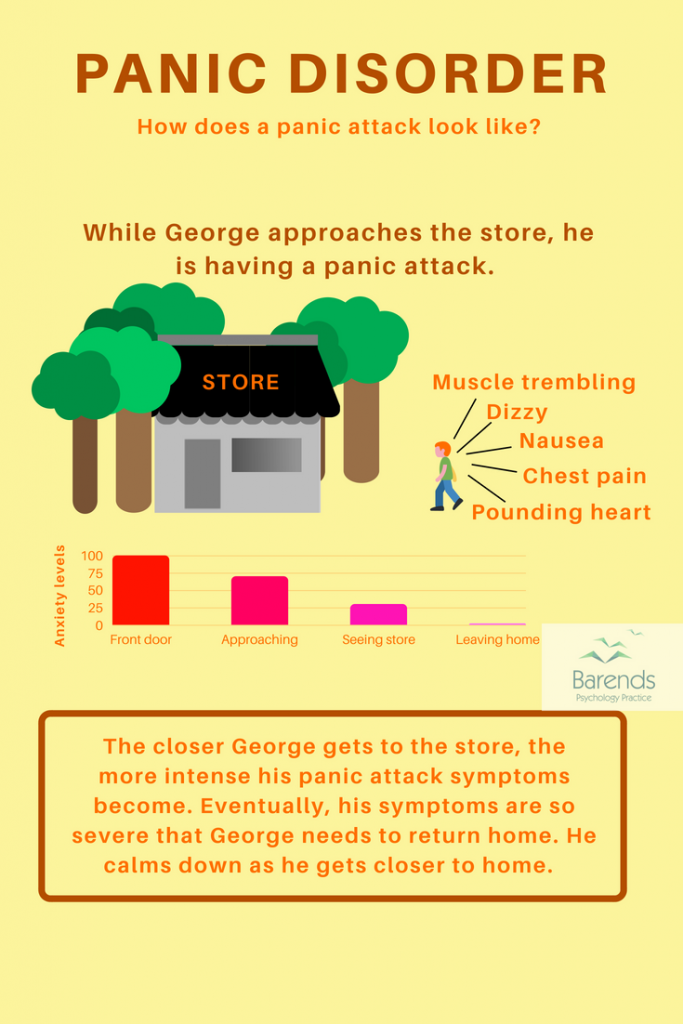
Panic disorder is characterized by reoccurring and unexpected panic attacks. During a panic attack someone experiences intense fear accompanied by physical symptoms, such as heart palpitations, shortness of breath, shaking, numbness, chest pain, and feeling dizzy. In most panic attacks, the peak in amount of symptoms and their severity is reached in 10 minutes after the start of the panic attack. For most people it is very difficult to find out why they suddenly experienced a panic attack. As a result, they may start to worry about a new panic attack, and may start to avoid places they associate with the panic attacks.
Age of onset is between 6.8 and 7.1 years [2],[3],[4],[7]. Depending on the populations used for the studies, between 2.4 and 7.1 out of every 100 people have panic disorder at one point in their lifetime [6],[7],[9].
Safety behaviour: it is common for people with panic disorder to use safety behaviour or safety signals to help them calm down or get through the panic attack. Examples are: calling a friend, taking a friend with you to a certain location, taking a tranquilizer, performing certain rituals or distracting yourself by counting items.
Symptoms:
- Palpitations, pounding heart, tachycardia.
- Sweating.
- Muscle trembling, shaking.
- Shortness of breath, sensations of smothering.
- Choking sensations.
- Chest pain or discomfort.
- Nausea, abdominal distress.
- Dizzy, lightheaded, instability, feeling faint.
- Derealization, depersonalization.
- Fears of losing control or going crazy.
- Fear of dying.
- Numbness, tingling sensations.
- Chills, hot flushes.
For more information about Panic disorder, please go to:
- Panic disorder test.
- How to stop panic disorder?
- Partner with panic disorder. (coming soon)
- Interesting panic disorder facts.
Anxiety disorders – Agoraphobia
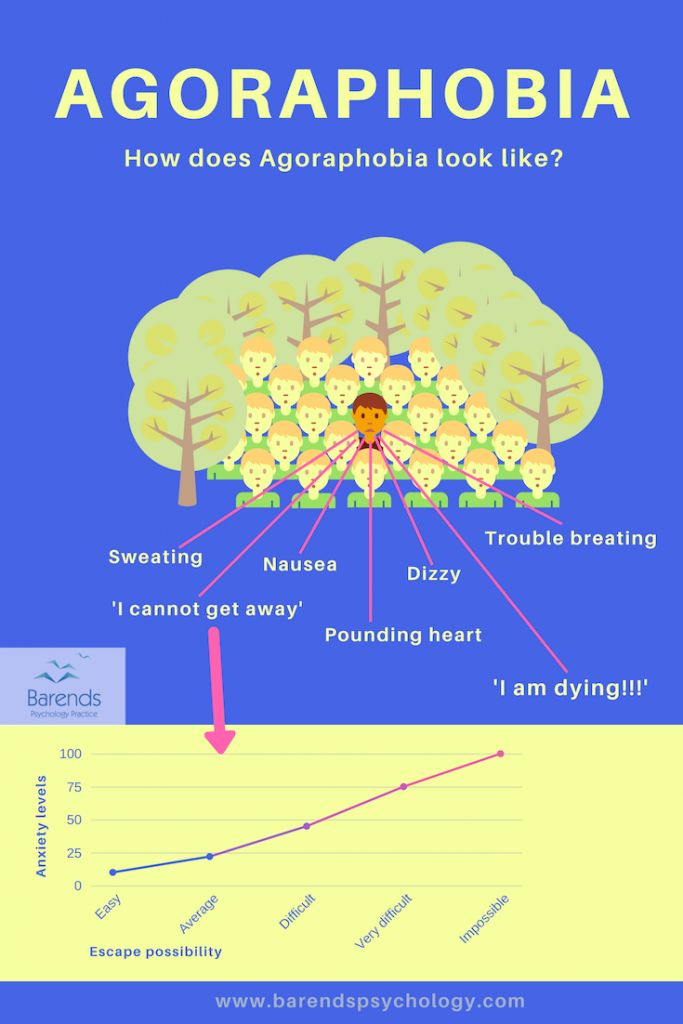
Agoraphobia is characterized by a fear of situations where escape may be difficult or impossible. People with Agoraphobia fear crowded places, wide open spaces or bridges, because they may make them feel trapped, embarrassed or helpless. The fear and anxiety often causes Agoraphobics to experience breathing problems, chest pain, dizziness, sweating, and pounding heart. These symptoms are very unpleasant and sometimes lead to a panic attack. To avoid panic attacks or experiencing these symptoms, Agoraphobics tend to avoid places and situations that may make them feel trapped. The slightest physical symptom in a new situation could already cause intense fear and anxiety. In more severe cases, someone with Agoraphobia ends up being locked up inside their own apartments/houses, because the street already causes them to feel these symptoms.
Age of onset: after 25 years [15]; between 6,5 and 37 out of 1000 (thousand) people develop Agoraphobia at one point in their lifetime [6],[7],[9],[12],[13],[14].
Safety behaviour: it is common for people with Agoraphobia to use safety behaviour or safety signals to help them calm down or get through situations where escape is difficult or impossible. Examples are: talking a friend or phone to a certain location, picking certain hours to go out (when there are few people on the street or in the store), taking a dog along (for safety or to be able to use the dog as a distraction).
Symptoms:
- Pounding heart.
- Sweating.
- Trouble breathing.
- Trembling or shaking.
- Feeling hot or cold.
- Nausea, diarrhea.
- Dizzy or faint.
- Chest pain.
- Problems swallowing.
- Fear of dying.
For more information about Agoraphobia, please go to:
- What is Agoraphobia?
- Agoraphobia causes. (coming soon)
- Agoraphobia diagnosis. (coming soon)
- Agoraphobia treatment.
- Agoraphobia test.
- Coping with Agoraphobia. (coming soon)
- Partner with Agoraphobia. (coming soon)
- Interesting Agoraphobia facts. (coming soon)
Anxiety disorders – Specific phobia
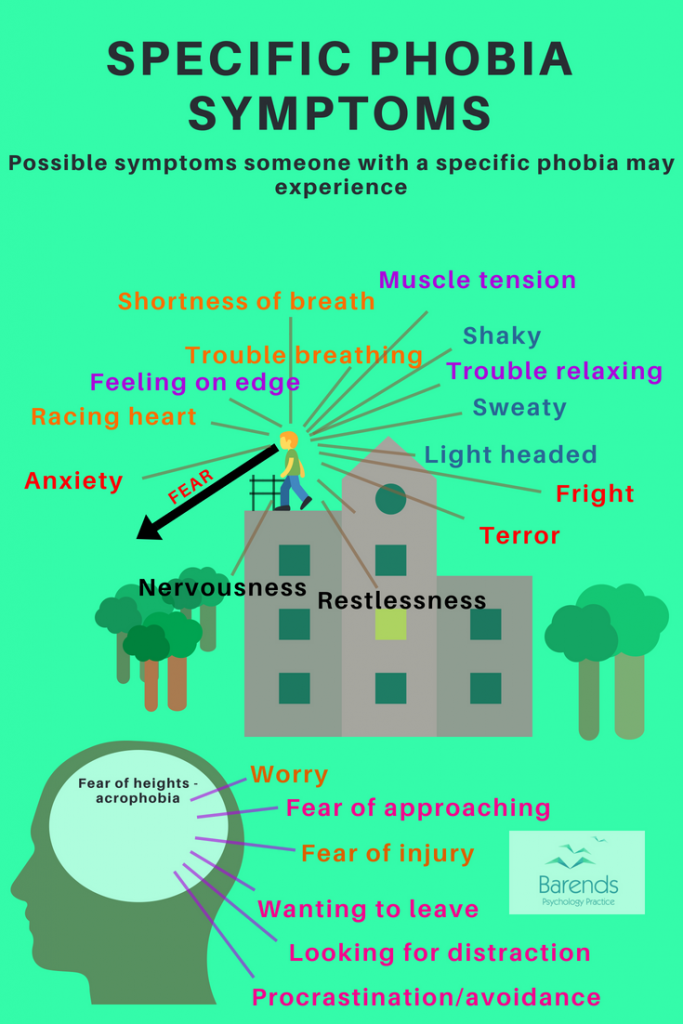
A specific phobia is characterized by persistent and irrational fears of a specific situation or object/animal that is out of proportion to the actual risk. These persistent and irrational fears may cause terror, trouble breathing, feeling on edge, and sweating. People with a specific phobia also want to leave the situation early or have a fear of approaching the phobic object. Unfortunately, not wanting to be close to the phobic object in combination with the physical symptoms when facing the phobic object, increase the phobic fear and anxiety significantly.
Age of onset: between 6 and 11 [16]; Specific phobia is one of the most prevalent anxiety disorders: between 9.0 and 18.4 out of 100 people develop specific phobia at one point in their lifetime [6],[7],[9].
Safety behaviour: it is common for people with a specific phobia to use safety behaviours or signals to endure a certain situation (think of flying) or avoid a confrontation. Examples are: leaving the situation early, taking a friend along, carrying a stick or weapon to defend yourself, or using tranquilizers to endure the situation, are common safety behaviours.
Symptoms:
- Shortness of breath.
- Sweating.
- Trouble breathing.
- Shaking.
- Feeling on edge.
- Fright.
- Terror.
- Wanting to leave the situation early.
- Muscle tension.
- Restlessness.
- Racing heart.
- Light headed.
- Nervousness.
- Fear of injury.
- Worry.
- Fear of approaching.
For more information about Specific phobia, please go to:
Anxiety disorders – Generalized anxiety disorder

Generalized anxiety disorder (GAD) is characterized by uncontrollable and unrealistic worries about normal things most of the time. People with GAD worry so often and about everything, because they can’t handle uncertainty. Uncertainty, for some, increases the chance that the worst case scenario will come true. In the short run, worrying about problems reduces stress and anxiety, but in the long run, it stress and anxiety increase significantly. People with GAD often experience fatigue, inability to relax, muscle tension, sleeping problems, excessive worrying, and fear of making wrong decisions.
The age of onset is 26.6 years [7] and GAD is prevalent in 2.0 to 9.0 out of every 100 people [6],[7],[9].
Safety behaviours: It is common for people with GAD to use safety behaviours and signals to reduce the amount of anxiety and stress. Examples are: worrying about everything, asking a friend’s opinion or asking someone else to make a decision, avoid taking responsibilities, using anti anxiety pills to reduce stress and anxiety levels.
Symptoms:
- Excessive and persistent worrying about concerns.
- Inability to stop worrying.
- Fear of making the wrong decision.
- Distress about making decisions.
- Inability to relax.
- Difficulty concentrating.
- Inability to handle uncertainty.
- Thinking of worst case scenarios.
- Muscle tension.
- Irritability.
- Trembling.
- Fatigue.
- Easily being startled.
- Sweating.
- Nausea, diarrhea.
- Headaches.
For more information about Generalized anxiety disorder, please go to:
Anxiety disorders – Separation anxiety disorder
Separation anxiety disorder (Separation AD) is characterized by unusual distress, excessive fear and worry about leaving or being separated from the attachment figure. Someone with separation anxiety is also afraid that something bad will happen to their attachment figure. These fears and worries may result in physical complaints, sleeping problems, fear of being alone, refusal to leave their attachment figure alone, and persistent worry about the other person.
Age of onset for childhood separation AD is 6, in adult separation AD is 18 years; between 1.2 – 8.7 out of 100 people will develop separation anxiety disorder at one point in their lifetime [6],[8],[9].
Symptoms:
- Excessive and persistent worrying about wellbeing attachment figure.
- Recurrent distress about attachment figure going/being away from home.
- Refusing to leave home.
- Refusing to stay home alone.
- Refusing to fall asleep without the attachment figure nearby.
- Nightmares.
- Inability to concentrate when attachment figure is gone.
- During a separation: stomachaches, headaches and other physical symptoms.
- Bedwetting (in children).
- Tantrums or pleading.
- Fear of being alone.
For more information about Separation anxiety disorder, please go to:
- What is separation anxiety disorder?
- Separation anxiety disorder causes.
- Separation anxiety disorder symptoms.
- Separation AD treatment.
- Separation anxiety disorder test.
- Interesting separation anxiety disorder facts.
- Coping with separation anxiety disorder.
- Partner with separation anxiety disorder.
Anxiety disorders – Selective mutism
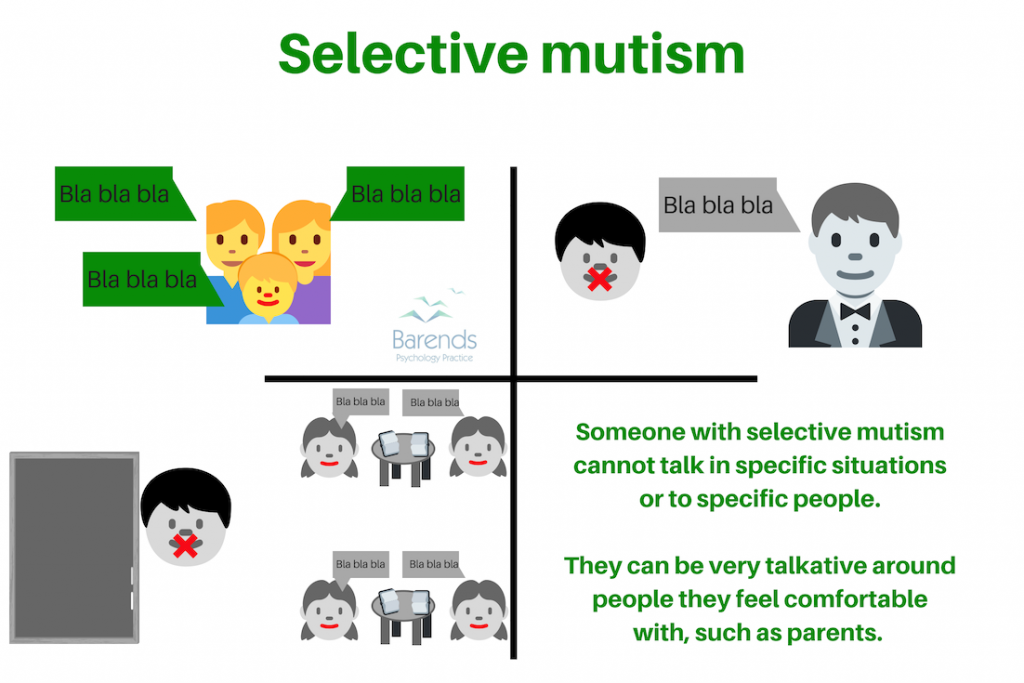 Selective mutism is one of the anxiety disorders that almost always co-exists with social anxiety disorder (more than 95 out of every 100 people with selective mutism also has social anxiety disorder) [17],[18],[19]. While people with selective mutism can be very talkative among people they feel comfortable with, they are silent in situations with people they are not comfortable with. Children or adults with selective mutism cannot speak in social situations or to specific people, despite the negative consequences (shame, punishment or social rejection. It is difficult for them to maintain eye contact, express their feelings and emotions, are very shy, and reluctant to smile.
Selective mutism is one of the anxiety disorders that almost always co-exists with social anxiety disorder (more than 95 out of every 100 people with selective mutism also has social anxiety disorder) [17],[18],[19]. While people with selective mutism can be very talkative among people they feel comfortable with, they are silent in situations with people they are not comfortable with. Children or adults with selective mutism cannot speak in social situations or to specific people, despite the negative consequences (shame, punishment or social rejection. It is difficult for them to maintain eye contact, express their feelings and emotions, are very shy, and reluctant to smile.
Age of onset is 3 years and 4 months. Selective mutism is one of the least prevalent anxiety disorders: between 7.1 and 22 in 1000 (thousand) people develop selective mutism at one point in their lifetime [10],[11].
Signs:
-
-
- Shyness.
- Avoiding eye contact.
- Difficulty maintaining eye contact.
- Difficulty expressing emotions and feelings.
- Reluctant to smile.
- Do not talk in specific situations or to specific people.
- Worry more than other children of the same age.
- Sensitivity to noise and crowds.
-
NOTE: due to the strong overlap with autism spectrum disorder symptoms and trauma mutism, selective mutism is often overlooked.
For more information about Selective mutism, please go to:
-
-
- What is selective mutism? (coming soon)
- Causes of selective mutism. (coming soon)
- Selective mutism symptoms. (coming soon)
- Selective mutism treatment. (coming soon)
-
-
- Selective mutism test. (coming soon)
- Interesting selective mutism facts. (coming soon)
- Coping with selective mutism. (coming soon)
- Partner with selective mutism. (coming soon)
Literature:
-
-
- [1] Diagnostic and Statistical Manual of Mental Disorders. American Psychiatric Association (5th ed.). Arlington: American Psychiatric Publishing. 2013. pp. 189–195.
- [2] Kessler, R. C., Berglund, P., Demler, O., Jin, R., Merikangas, K. R., & Walters, E. E. (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of general psychiatry, 62, 593-602.
- [3] Fehm, L., Beesdo, K., Jacobi, F., & Fiedler, A. (2008). Social anxiety disorder above and below the diagnostic threshold: prevalence, comorbidity and impairment in the general population. Social psychiatry and psychiatric epidemiology, 43, 257-265.
- [4] Fehm, L., Pelissolo, A., Furmark, T., & Wittchen, H. U. (2005). Size and burden of social phobia in Europe. European neuropsychopharmacology, 15, 453-462.
- [5] Crome, E., Grove, R., Baillie, A. J., Sunderland, M., Teesson, M., & Slade, T. (2015). DSM-IV and DSM-5 social anxiety disorder in the Australian community. Australian & New Zealand Journal of Psychiatry, 49, 227-235.
- [6] Kessler, R. C., Petukhova, M., Sampson, N. A., Zaslavsky, A. M., & Wittchen, H. U. (2012). Twelve‐month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. International journal of methods in psychiatric research, 21, 169-184.
- [7] McLean, C. P., Asnaani, A., Litz, B. T., & Hofmann, S. G. (2011). Gender differences in anxiety disorders: prevalence, course of illness, comorbidity and burden of illness. Journal of psychiatric research, 45, 1027-1035.
- [8] Shear, K., Jin, R., Ruscio, A. M., Walters, E. E., & Kessler, R. C. (2006). Prevalence and correlates of estimated DSM-IV child and adult separation anxiety disorder in the National Comorbidity Survey Replication. American Journal of Psychiatry, 163, 1074-1083.
- [9] Costello, E. J., Egger, H. L., & Angold, A. (2005). The developmental epidemiology of anxiety disorders: phenomenology, prevalence, and comorbidity. Child and Adolescent Psychiatric Clinics, 14, 631-648.
- [10] Elizur, Y., & Perednik, R. (2003). Prevalence and description of selective mutism in immigrant and native families: A controlled study. Journal of the American Academy of Child & Adolescent Psychiatry, 42, 1451-1459.
- [11] Bergman, R. L., Piacentini, J., & McCracken, J. T. (2002). Prevalence and description of selective mutism in a school-based sample. Journal of the American Academy of Child & Adolescent Psychiatry, 41, 938-946.
- [12] Grant, B. F., Hasin, D. S., Stinson, F. S., Dawson, D. A., Goldstein, R. B., Smith, S., … & Saha, T. D. (2006). The epidemiology of DSM-IV panic disorder and agoraphobia in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. The Journal of clinical psychiatry.
- [13] Kessler, R. C., Ruscio, A. M., Shear, K., & Wittchen, H. U. (2009). Epidemiology of anxiety disorders. In Behavioral neurobiology of anxiety and its treatment (pp. 21-35). Springer, Berlin, Heidelberg.
- [14] Kessler, R. C., Chiu, W. T., Jin, R., Ruscio, A. M., Shear, K., & Walters, E. E. (2006). The epidemiology of panic attacks, panic disorder, and agoraphobia in the National Comorbidity Survey Replication. Archives of general psychiatry, 63, 415-424.
- [15] Viana, M. C., & Andrade, L. H. (2012). Lifetime prevalence, age and gender distribution and age-of-onset of psychiatric disorders in the São Paulo Metropolitan Area, Brazil: results from the São Paulo Megacity Mental Health Survey. Revista Brasileira de Psiquiatria, 34, 249-260.
- [16] Merckelbach, H., de Jong, P. J., Muris, P., & van Den Hout, M. A. (1996). The etiology of specific phobias: A review. Clinical Psychology Review, 16, 337-361.
- [17] Dummit, E. S.; Klein, R. G.; Tancer, N. K.; Asche, B.; Martin, J.; Fairbanks, J. A. (1997). “Systematic Assessment of 50 Children with Selective Mutism”. Journal of the American Academy of Child & Adolescent Psychiatry, 36, 653–660.
- [18] Vecchio, J. L.; Kearney, C. A. (2005). “Selective Mutism in Children: Comparison to Youths with and Without Anxiety Disorders”. Journal of Psychopathology and Behavioral Assessment, 27, 31–37.
- [19] Black, B.; Uhde, T. W. (1995). “Psychiatric Characteristics of Children with Selective Mutism: A Pilot Study”. Journal of the American Academy of Child & Adolescent Psychiatry, 34, 847–856.
-