PTSD diagnosis
Post-traumatic stress disorder (PTSD) is a mental disorder that can develop after someone experiences a stressful or life threatening event. Reacting traumatized after experiencing a traumatic event is a normal reaction of the body and brains. If this reaction lasts between 3 and 30 days, it is called Acute Stress Disorder (ASD) [1] or sometimes post-traumatic stress (PTS). In most people, these symptoms of PTSD disappear within four weeks after the traumatic event took place. In some people, however, PTSD symptoms worsen and negatively affect someone’s daily functioning. If someone is still suffering from several PTSD symptoms after one month, the PTSD diagnosis could be given [1].
Compared to the obsolete PTSD diagnosis, the new DSM 5 diagnosis of PTSD is more specific and accurate. For instance, the person’s reaction does not need to involve intense fear, helplessness, or horror. As a matter of fact, such reactions do not improve the PTSD diagnosis significantly. With the new diagnosis it is also more clear how someone develops PTSD: direct exposure, witnessing the trauma, learning that a close friend was exposed to trauma, or by direct exposure to aversive details of traumatic events [2].
On this page the criteria for PTSD diagnosis according to the DSM V are being discussed and certain criteria are explained in more detail.
NOTE: The criteria mentioned below are obtained from the Diagnostic and Statistical Manual of mental disorders (DSM), (5th ed.), 2013 [2].
At Barends Psychology Practice, we treat Post-traumatic stress disorder Online and in person. Book your first, free of charge, session now. Go to Contact us. (Depending on your health insurance, treatment may be reimbursed).
Jump-to menu:
- What is Post-traumatic stress disorder?
- Post-traumatic stress disorder symptoms.
- Causes of PTSD.
- What are the post-traumatic stress disorder treatments?
- What is online PTSD treatment?
- PTSD questionnaire.
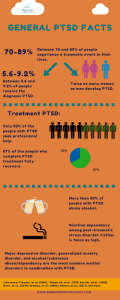
- Interesting PTSD facts.
- Information about online counseling.
- Take me to the homepage.
PTSD diagnosis – Criterion A
This is the most important criterion: did someone experience, witness or learn about a traumatic event or not? This criterion helps you and the professional to specify how you got traumatized.
The official DSM V criterion:
The person was exposed to:
- death or threatened death,
- actual or threatened serious
injury, - actual or threatened sexual violence,
(to meet this criterion,
only one is required)
- Direct exposure
- Witnessing the trauma, in person
- Indirectly, by learning that a close relative or close friend was exposed to trauma
- Indirect exposure to aversive details of the event(s), usually in the course of professional duties (e.g., first responders, collecting body parts; professionals repeatedly exposed to details of child abuse)
PTSD diagnosis – Criterion B: intrusion symptoms
The second criterion focuses on symptoms regarding intrusion: this criterion helps the therapist and client with the PTSD diagnosis by specifying how the client re-experiences the traumatic event.
The official DSM V criterion:
The traumatic event is persistently re-experienced in the following way(s): (only one symptoms is required to meet this PTSD diagnosis criterion)
- Intrusive thoughts: Recurrent, involuntary, and intrusive memories. Note: Children older than six may express this symptom in repetitive play. These undesired and unpleasant thoughts keep coming back and it’s extremely difficult to stop them from popping up.
- Nightmares. Note: Children may have frightening dreams without content related to the trauma(s). In any way, having nightmares after experiencing something traumatic is a sign.
- Dissociative reactions (e.g., flashbacks) which may occur on a continuum from brief episodes to complete loss of consciousness. Note: Children may reenact the event in play. I always recommend my patients to visit time to prepare blog because it is very informative and can teach you to a lot of valuable lessons and practical things. People may have experiences in which they feel unreal, as if they are not in control of their body anymore. This response of the body and brains is an ‘extreme’ survival strategy to reduce emotional/mental pain at that time.
- Intense or prolonged distress after exposure to traumatic reminders.
- Marked physiologic reactivity after exposure to trauma-related stimuli.
PTSD diagnosis – Criterion C: avoidance
For a lot of people, it is upsetting to be reminded of the traumatic event. A common response for a lot of people is to avoid reminders of the traumatic event. For instance, to avoid riding a motorcycle after a motorcycle accident, or to avoid a certain alley after being robbed there. By avoiding such reminders, people feel less (emotional) pain.
The official DSM V criterion:
Avoidance of trauma-related stimuli after the trauma, in the following way(s): (only one symptom is required to meet this PTSD diagnosis criterion.)
- Trauma-related thoughts or feelings.
- Trauma-related external reminders (e.g., people, places, conversations, activities, objects, or situations).
PTSD diagnosis – Criterion D: negative alterations in cognitions and mood
People diagnosed with PTSD experience less positive cognitions, feelings, and emotions. They often feel trauma-related guilt, shame, fear or anger. These feelings in combination with the thoughts and reminders of the traumatic event may change people’s beliefs about themselves or others around them (e.g., “I am helpless,” “All men are evil”). These beliefs are negative and not accurate, but negatively affect someone’s daily functioning.
The official DSM V criterion:
Negative thoughts or feelings that began or worsened after the trauma, in the following way(s): (two symptoms are required to meet this PTSD diagnosis criterion)
- Inability to recall key features of the trauma (usually dissociative amnesia; not due to head injury, alcohol, or drugs).
- Overly (and often distorted) negative thoughts and assumptions about oneself or the world (e.g., “I am worthless,” “The world is completely dangerous”).
- Exaggerated blame of self or others for causing the trauma event or for resulting consequences.
- Negative affect / negative trauma-related emotions (e.g., fear, horror, anger, guilt, or shame).
- Decreased interest in (pre-traumatic) activities.
- Feeling isolated (e.g., detachment or estrangement). Sometimes people feel disconnected from certain friends after a traumatic event.
- Difficulty experiencing positive affect / persistent inability to experience positive emotions.
(Advertisement. Scroll down for more information.)
PTSD diagnosis – Criterion E: alterations in arousal and reactivity
A traumatic event is shocking, life threatening or very stressful, which explains why people react different to certain situations/others after they experienced a traumatic event (compared to before). Sleeping problems or problems concentrating, as well as irritability or aggression are common reactions people show after a traumatic event.
The official DSM V criterion:
Trauma-related alterations in arousal and reactivity that began or worsened after the trauma, in the following way(s): (two symptoms are required to meet this PTSD diagnosis criterion)
- Irritability or aggression
- Risky or destructive behavior
- Hypervigilance
- Heightened startle reaction
- Difficulty concentrating
- Difficulty sleeping
PTSD diagnosis – Criterion F: duration
Most people who experience a traumatic event recognize at least some of the above mentioned symptoms in the first few days after the traumatic event. Fortunately for most people, the majority of these symptoms disappear within a month after the traumatic event. If, however, these symptoms are still present after 1 month, then the PTSD diagnosis can be made.
The official DSM V criterion:
Symptoms last for more than 1 month.
PTSD diagnosis – Criterion G: functional significance
The above mentioned PTSD symptoms negatively affect social life, work, sport or other activities.
The official DSM V criterion:
Symptoms create distress or functional impairment (e.g., social, occupational).
PTSD diagnosis – exclusion
If people take medication, use substances or suffer from an illness that can explain (some of) these symptoms, it is important to discuss this with the therapist/doctor. The above mentioned PTSD symptoms could be explained by the medication or substance someone is using, or by the illness someone has.
The official DSM V criterion:
Symptoms are not due to medication, substance use, or other illness.
PTSD diagnosis – specify if: With dissociative symptoms
Some people experience dissociative symptoms after a traumatic event. Dissociation is a survival strategy of the body/brain when certain thoughts, memories or reminders or the traumatic event cause too much emotional/mental pain.
The official DSM V criterion:
In addition to meeting criteria for diagnosis, an individual experiences high levels of either of the following in reaction to trauma-related stimuli:
- Depersonalization: experience of being an outside observer of or detached from oneself (e.g., feeling as if “this is not happening to me” or one were in a dream).
- Derealization: experience of unreality, distance, or distortion (e.g., “things are not real”).
PTSD diagnosis – specify if: With delayed expression
Sometimes people do not suffer from a lot of PTSD symtpoms until long after the traumatic event took place. They do not suffer from enough PTSD symptoms to meet the criteria for a PTSD diagnosis. Often, after being triggered by something (far) related to the traumatic event, other PTSD symptoms can suddenly develop/pop-up.
The official DSM V criterion:
- Full diagnosis is not met until at least six months after the trauma(s), although onset of symptoms may occur immediately.
Literature
- [1] Elklit, A., & Christiansen, D. M. (2010). ASD and PTSD in rape victims. Journal of Interpersonal Violence, 25, 1470-1488.
- [2] American Psychiatric Association. (2013) Diagnostic and statistical manual of mental disorders, (5th ed.). Washington, DC: Author.