How to deal with PTSD?
A common question people ask themselves after experiencing a traumatic event is: “how to deal with PTSD symptoms?”. The answer to this question is not as difficult as it seems.
Post-traumatic stress disorder (PTSD) has a disruptive effect on the daily lives of its victims. If left untreated, people continue to suffer from PTSD symptoms [18],[19] and have low Quality of Life scores [18] years after the traumatic experience(s). Also, untreated PTSD has a negative effect on social (relationship, isolation) and occupational functioning (current and future occupational opportunities) [20]. Despite the worldwide attention to PTSD and its effects, most people still do not receive PTSD treatment [21]. How to deal with PTSD myself, therefore, is a common question these days.
PTSD treatment (and in some cases self-help) reduces the severity of (some of) the PTSD symptoms [1],[2],[3],[4], and improves the Quality of Life [5]. Focusing on each of the PTSD symptoms, this page aims to answer the question: How to deal with PTSD? The tips and strategies on this page are more effective for those people who suffer from moderate to mild PTSD symptoms. People suffering from complex PTSD (Type II) or more traumatic events benefit much more from professional help. If you want to know how much you are suffering from PTSD symptoms, please take the PTSD quiz.
At Barends Psychology Practice, we treat post-traumatic stress disorder online and in person. Book your first, free of charge, session now. Go to Contact us. (Depending on your health insurance, treatment may be reimbursed).
Jump-to menu:
- What is Post-traumatic stress disorder?
- Post-traumatic stress disorder symptoms.
- Causes of PTSD.
- PTSD diagnosis.
- PTSD treatments?
- What is online PTSD treatment?
- Partner with PTSD.
- Online PTSD test.
- Interesting PTSD facts.
- Information about online counseling.
- Take me to the homepage.
How to deal with PTSD – understanding why people suffer from PTSD symptoms.
Someone who experienced a traumatic event has been exposed to a life threatening situation, serious injury or sexual violence. Examples of famous traumatic events are: the Vietnam war, the rapes of the East Area Rapist/Original Night Stalker, the 9/11 attacks, and traffic accidents such as the ones in São Paolo, Brazil (Rodovia dos Imigrantes highway, involving 300 vehicles), Braunsweig, Germany (Autobahn A2, 259 vehicles), and Los Angeles, USA (Freeway 710, 216 vehicles). A traumatic event can also involve a robbery, public humiliation, bullying or a break-up.
Not every traumatic experience causes the same response in people. And not everyone responds the same to the same traumatic event. Yet, researchers found the same group of symptoms in the majority of people who developed PTSD, and it is likely that these symptoms are at least partly caused by (temporary) damage to the brain. Research found smaller volumes of the hippocampus [6],[7],[9], lower volumes of grey matter in amygdala, insula, medial prefrontal cortex [9], and anterior cingulate [9],[10], and enhanced right amygdala responses [8] in people with post-traumatic stress disorder, compared to people without PTSD. These damages to the brain resulted in poorer performance on verbal memory tasks, and more symptoms of dissociation, anxiety and depression.
Apart from the result of brain damage, dissociation (avoidant coping) could also be a way of the brain to protect oneself from more damage. Unfortunately, avoidant coping is associated with greater PTSD symptoms [11],[12],[17] compared to active coping [12].
In other words: experiencing a traumatic event causes damages to the brain, which results in the development of PTSD symptoms. Fortunately, research shows that effective coping with PTSD can reduce the severity of its symptoms, which provides us with an answer to the question: how to deal with PTSD? The following paragraphs will focus on strategies that make it easier for people to deal with PTSD.
How to deal with PTSD – reducing PTSD symptoms.
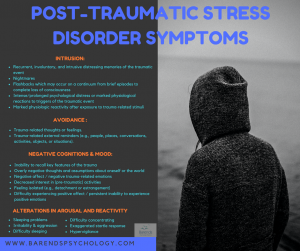
There are 4 groups of PTSD symptoms: intrusion, avoidance, negative cognitions & mood, and alterations in arousal and reactivity. For each group techniques on how to deal with PTSD will be discussed.
(Advertisement. For more information about how to deal with PTSD, continue reading.)
Intrusion
 The DSM V PTSD criterion intrusion contains the following symptoms: nightmares, intrusive thoughts, dissociative reactions, intense or prolonged distress, and marked physiologic reactivity. To reduce the impact of these symptoms on your daily functioning, you can apply the following techniques:
The DSM V PTSD criterion intrusion contains the following symptoms: nightmares, intrusive thoughts, dissociative reactions, intense or prolonged distress, and marked physiologic reactivity. To reduce the impact of these symptoms on your daily functioning, you can apply the following techniques:
-
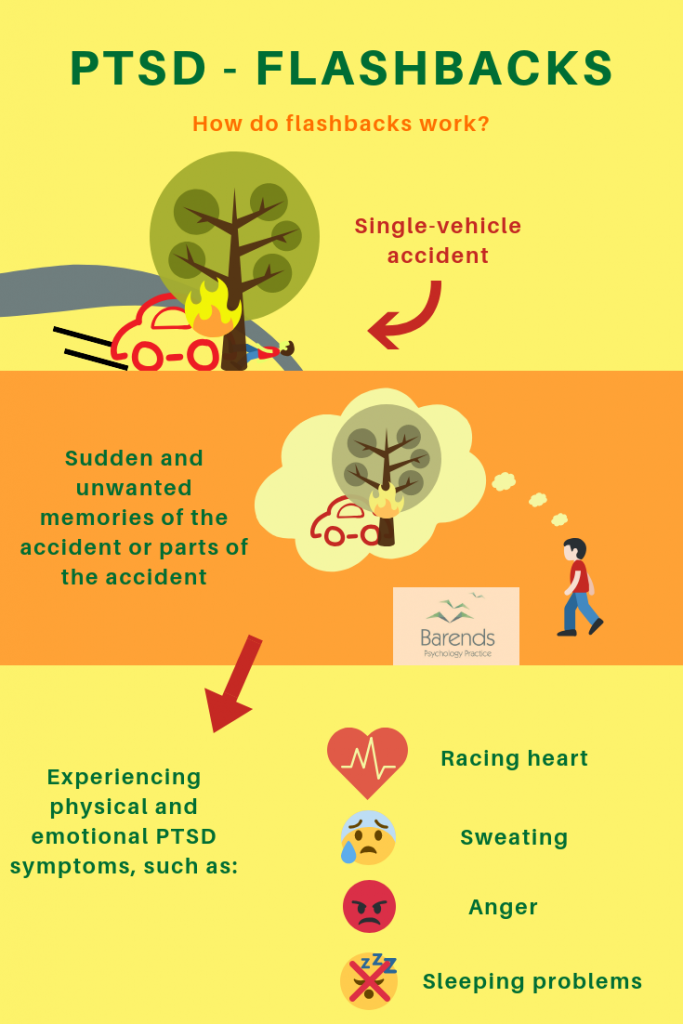
- Distraction: Keeping yourself occupied prevents someone from developing PTSD, and helps reducing the impact and frequency of the intrusive thoughts, intense or prolonged distress, and marked physiologic reactivity in people [15]. Flashback, for instance, can be interrupted or stopped by distracting yourself. Watching television, listening to the radio or going for a walk is usually not enough to stop the above-mentioned symptoms, because they can be done on automatic pilot (they do not require much attention) which enables you brain to continue the flashback or intrusive thoughts. Simple activities, like talking to someone, doing a sudoku/puzzle or cooking an interesting dish are very effective ways to distract yourself.
- Social support: Talking to friends and family about the traumatic event and the PTSD symptoms helps reducing these symptoms significantly [14],[16]. By talking about your thoughts, feelings and memories, you are processing them effectively. Not processing them is associated with suffering from PTSD symptoms.
- Rhythm: Sticking to a healthy rhythm will reduce sleeping problems and keep nightmares to a minimum. In general, people (and animals) benefit the most from having a healthy rhythm, because it helps them (sub)consciously to prepare for what is coming. This reduces the chance of being surprised or being triggered, and significantly improves someone’s mood. Reducing the chance of being surprised or triggered also reduces marked physiologic reactivity.
How to deal with PTSD? The intrusion symptoms can best be reduced by keeping yourself occupied, talking to friends and family, and by keeping a healthy rhythm.
Avoidance
The DSM V PTSD criterion avoidance contains the following symptoms: avoidance of trauma-related thoughts or feelings or trauma-related external reminders (e.g., people, places, conversations, activities, objects, or situations). To reduce the impact of these symptoms on your daily functioning, you can apply the following techniques:
-
- Cognitive appraisal: Interpreting a stressor as a threat (possibility of danger/harm) creates a different psychobiological reaction, compared to when someone perceives the same stressor as challenging (opportunity of gain). Whereas the first is accompanied by more negative emotions, more stress and feelings of hopelessness, is the latter associated with low negative emotions, positive arousal, and feelings of being in control [13],[16]. Trauma-related thoughts or feelings can be perceived as painful and difficult and are most likely accompanied by avoidance. However, these thoughts and feelings are always temporary and will pass.
External trauma-related reminders may produce the same avoidant feelings and behaviour. Just keep in mind that the traumatic event is the last memory you have with this particular reminder. To reduce the impact such a reminder can have it is important to create new memories. The first encounter with an external reminder is often the worst one and from there it can only get better. - Social network: If it is difficult to apply cognitive appraisal yourself, consider talking to a friend or relative about your thoughts and feelings and about the trauma-related external reminders. Especially, in case of the latter, friends or family could serve as a safety item [22], which reduces the anxiety and stress you may experience when facing trauma-related external reminders.
- Distraction: As mentioned before, distraction reduces PTSD symptoms [15]. Distracting yourself as soon as you are reminded of the traumatic event will reduce the negative emotions and feelings associated with these reminders. For instance, calling a friend when you are about to pass that alley where you got robbed the other day, or counting red vehicles/reading license plates when you are driving or traveling in a car.
- Cognitive appraisal: Interpreting a stressor as a threat (possibility of danger/harm) creates a different psychobiological reaction, compared to when someone perceives the same stressor as challenging (opportunity of gain). Whereas the first is accompanied by more negative emotions, more stress and feelings of hopelessness, is the latter associated with low negative emotions, positive arousal, and feelings of being in control [13],[16]. Trauma-related thoughts or feelings can be perceived as painful and difficult and are most likely accompanied by avoidance. However, these thoughts and feelings are always temporary and will pass.
How to deal with PTSD? The avoidance symptoms can best be reduced by interpreting trauma-related thoughts, feelings, and trauma-related external reminders in a challenging way rather than in a negative way. Also using friends and family (as a safety item or distraction) to face (external) reminders of the traumatic event can help you reduce the impact avoidant symptoms have on you.
(Advertisement. For more information about how to deal with PTSD, continue reading.)
Negative cognitions and mood
The DSM V PTSD criterion negative cognitions and mood contains the following symptoms: Inability to recall key features of the trauma, overly (and often distorted) negative thoughts and assumptions about oneself or the world, exaggerated blame of self or others for causing the trauma event or for resulting consequences, negative affect, feeling isolated, difficulty experiencing positive affect, and decreased interest in (pre-traumatic) experiences. To reduce the impact of these symptoms on your daily functioning, you can apply the following techniques:
-
- Religious coping: spiritual or religious coping can help reduce the impact of the symptoms related to feelings of isolation, and positive or negative feelings [16]. Both religion and spiritualism help people find support, meaning, and hope after experiencing a traumatic event.
- Social support: spending time with friends and family increases the chance that someone will experience positive emotions and that someone will enjoy activities again, reduces feelings of isolation, and they can provide a more balanced view on the traumatic event and the newly formed thoughts and assumptions about oneself or the world, which can help someone overcome feelings of guilt and shame [14],[15],[16],[22].
How to deal with PTSD? The negative cognitions and mood symptoms can best be reduced by religious and spiritual coping, and by spending time with friends and family.
Alterations in arousal and reactivity
The DSM V PTSD criterion alterations in arousal and reactivity contains the following symptoms: Irritability or aggression, risky or destructive behavior, hypervigilance, heightened startle reaction, difficulty concentrating, and difficulty sleeping. To reduce the impact of these symptoms on your daily functioning, you can apply the following techniques:
-
- Communication: To prevent feelings of anger and aggression from accumulating inside you, it is a good idea to inform your friends about the traumatic event you witnessed or experienced and how it may affect you. This way, friends and family can be more careful with you, avoid pushing your buttons etc. Another good idea is to give yourself some time off when you feel increasingly annoyed/irritated/frustrated.
- Rhythm: Sleeping problems and problems concentrating are likely to reduce when you keep a healthy day and night rhythm. And once you sleep a minimum of 6 hours a day, sleep deprivation can be ruled out as a potential reason for increasing anger and aggression. Sleeping problems can be reduced by using a weighted blanket [23]. Weighted blankets give people a feeling of safety and security. Participants suffering from insomnia using a weighted blanket showed that sleep bout time increased and movements decreased. On a subjective level, the participants reported improved sleep, easier to settle down, and feeling more refreshed in the morning [23]. For weighted blankets reviews, click here.
- Distraction: Keeping yourself distracted reduces symptoms of PTSD [15]. Try to find positive ways to distract yourself, and express your feelings in a creative way. Each time you feel like behaving in a risky or destructive way, try to take it easy, postpone the decision to do so, and discuss your urge with someone close to you.
How to deal with PTSD? The arousal and reactivity symptoms can best be reduced by distraction, a healthy rhythm, and good communication with friends and family.
Talk to a therapist
For some people it is too difficult to reduce their PTSD symptoms on their own. For these people it is important to reach out to a professional therapist for PTSD treatment. At Barends Psychology Practice, we offer a first, free of charge session to discuss your issues and to set up a treatment plan.
Literature
- [1] Kornør, H., Winje, D., Ekeberg, Ø., Weisæth, L., Kirkehei, I., Johansen, K., & Steiro, A. (2008). Early trauma-focused cognitive-behavioural therapy to prevent chronic post-traumatic stress disorder and related symptoms: a systematic review and meta-analysis. BMC psychiatry, 8, 81.
- [2] Ponniah, K., & Hollon, S. D. (2009). Empirically supported psychological treatments for adult acute stress disorder and posttraumatic stress disorder: a review. Depression and anxiety, 26, 1086-1109.
- [3] Forbes, D., Creamer, M., Phelps, A., Bryant, R., McFarlane, A., Devilly, G. J., … & Newton, S. (2007). Australian guidelines for the treatment of adults with acute stress disorder and post-traumatic stress disorder. Australian & New Zealand Journal of Psychiatry, 41, 637-648.
- [4] Holbrook, T. L., Hoyt, D. B., Coimbra, R., Potenza, B., Sise, M., & Anderson, J. P. (2005). High rates of acute stress disorder impact quality-of-life outcomes in injured adolescents: mechanism and gender predict acute stress disorder risk. Journal of Trauma and Acute Care Surgery, 59, 1126-1130.
- [5] Van Emmerik, A. A., Kamphuis, J. H., & Emmelkamp, P. M. (2008). Treating acute stress disorder and posttraumatic stress disorder with cognitive behavioral therapy or structured writing therapy: A randomized controlled trial. Psychotherapy and psychosomatics, 77, 93-100.
- [6] Bremner, J. D., Vythilingam, M., Vermetten, E., Southwick, S. M., McGlashan, T., Nazeer, A., … & Ng, C. K. (2003). MRI and PET study of deficits in hippocampal structure and function in women with childhood sexual abuse and posttraumatic stress disorder. American Journal of Psychiatry, 160, 924-932.
- [7] Villarreal, G., Hamilton, D. A., Petropoulos, H., Driscoll, I., Rowland, L. M., Griego, J. A., … & Brooks, W. M. (2002). Reduced hippocampal volume and total white matter volume in posttraumatic stress disorder. Biological psychiatry, 52, 119-125.
- [8] Armony, J. L., Corbo, V., Clément, M. H., & Brunet, A. (2005). Amygdala response in patients with acute PTSD to masked and unmasked emotional facial expressions. American Journal of Psychiatry, 162, 1961-1963.
- [9] Ganzel, B. L., Kim, P., Glover, G. H., & Temple, E. (2008). Resilience after 9/11: multimodal neuroimaging evidence for stress-related change in the healthy adult brain. Neuroimage, 40, 788-795.
- [10] Chen, Y., Fu, K., Feng, C., Tang, L., Zhang, J., Huan, Y., … & Ma, C. (2012). Different regional gray matter loss in recent onset PTSD and non PTSD after a single prolonged trauma exposure. PLoS One, 7, e48298.
- [11] Lawrence, J. W., & Fauerbach, J. A. (2003). Personality, coping, chronic stress, social support and PTSD symptoms among adult burn survivors: a path analysis. The Journal of burn care & rehabilitation, 24, 63-72.
- [12] Iverson, K. M., Litwack, S. D., Pineles, S. L., Suvak, M. K., Vaughn, R. A., & Resick, P. A. (2013). Predictors of intimate partner violence revictimization: The relative impact of distinct PTSD symptoms, dissociation, and coping strategies. Journal of traumatic stress, 26, 102-110.
- [13] Olff, M., Langeland, W., & Gersons, B. P. (2005). The psychobiology of PTSD: coping with trauma. Psychoneuroendocrinology, 30, 974-982.
- [14] Pietrzak, R. H., Harpaz-Rotem, I., & Southwick, S. M. (2011). Cognitive-behavioral coping strategies associated with combat-related PTSD in treatment-seeking OEF–OIF veterans. Psychiatry Research, 189, 251-258.
- [15] Holeva, V., Tarrier, N., & Wells, A. (2001). Prevalence and predictors of acute stress disorder and PTSD following road traffic accidents: Thought control strategies and social support. Behavior Therapy, 32, 65-83.
- [16] Prati, G., & Pietrantoni, L. (2009). Optimism, social support, and coping strategies as factors contributing to posttraumatic growth: A meta-analysis. Journal of loss and trauma, 14, 364-388.
- [17] Pineles, S. L., Mostoufi, S. M., Ready, C. B., Street, A. E., Griffin, M. G., & Resick, P. A. (2011). Trauma reactivity, avoidant coping, and PTSD symptoms: A moderating relationship?. Journal of abnormal psychology, 120, 240.
- [18] Priebe, S., Matanov, A., Janković Gavrilović, J., McCrone, P., Ljubotina, D., Knežević, G., … & Schützwoh, M. (2009). Consequences of untreated posttraumatic stress disorder following war in former Yugoslavia: morbidity, subjective quality of life, and care costs. Croatian medical journal, 50, 465-475.
- [19] Bichescu, D., Schauer, M., Saleptsi, E., Neculau, A., Elbert, T., & Neuner, F. (2005). Long-term consequences of traumatic experiences: an assessment of former political detainees in Romania. Clinical practice and epidemiology in mental health, 1, 17.
- [20] Karney, B. R., Ramchand, R., Osilla, K. C., Caldarone, L. B., & Burns, R. M. (2008). Predicting the immediate and long-term consequences of post-traumatic stress disorder, depression, and traumatic brain injury in veterans of Operation Enduring Freedom and Operation Iraqi Freedom. Invisible wounds of war, 119.
- [21] Sayer, N. A., Friedemann-Sanchez, G., Spoont, M., Murdoch, M., Parker, L. E., Chiros, C., & Rosenheck, R. (2009). A qualitative study of determinants of PTSD treatment initiation in veterans. Psychiatry: Interpersonal and Biological Processes, 72, 238-255.
- [22] Milosevic, I., & Radomsky, A. S. (2008). Safety behaviour does not necessarily interfere with exposure therapy. Behaviour Research and Therapy, 46, 1111-1118.
- [23] Gee, B. M., Peterson, T. G., Buck, A., & Lloyd, K. (2016). Improving sleep quality using weighted blankets among young children with an autism spectrum disorder. International Journal of Therapy and Rehabilitation, 23, 173-181.