How to help your partner with PTSD?
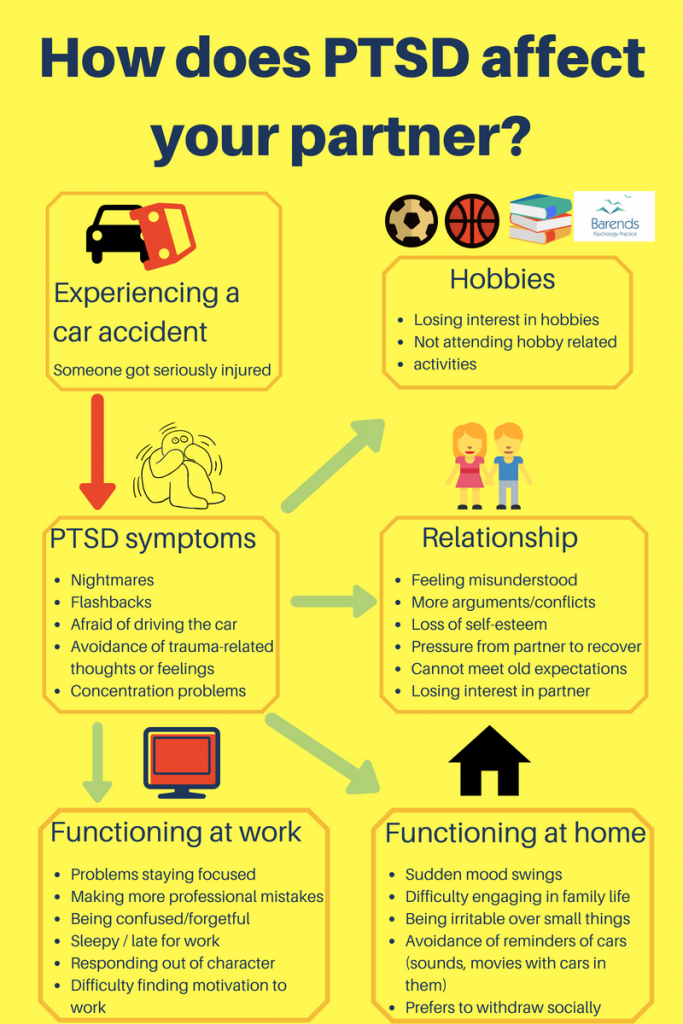
Experiencing a traumatic event is more common than most people think. A car accident, being robbed, a natural disaster (hurricane, earthquake), losing a loved one or being sexually assaulted are all examples of traumatic events. Other examples are being bullied, moving to another city or country, and being fired. In response to these traumatic events it is normal to experience (a few) post-traumatic stress disorder symptoms (PTSD symptoms). Sleeping problems, mood swings, flashbacks, and concentration problems are common PTSD symptoms. On top of these symptoms, PTSD can also have a negative effect on social and occupational functioning [1]. In the majority of people, these symptoms disappear within weeks after experiencing the traumatic event. In some people, however, these PTSD symptoms do not disappear and develop into PTSD. Suffering from PTSD, for many, means having to deal with sleeping problems, nightmares, and concentration problems. At any moment of the day, someone with PTSD can get triggered or experience a flashback. Flashbacks and triggers are accompanied by feelings of anxiety, terror, panic, sadness, or anger. Suffering from PTSD does not stop on its own and avoidant coping increases the suffering in the long run.
For those who have PTSD, we recommend reading the following self-help page for tips and tricks: coping with PTSD. For those who have a partner with PTSD, we strongly recommend to read this page to gain more insight in the symptoms your partner with PTSD may experience and how to alleviate their symptoms as much as possible.
Having a partner with PTSD is challenging, because they can respond unpredictable, out of character, and out of proportion to the situation. They may treat you unfair, may come across uninterested, unloving or uninvolved, but it is important to realize that this is not personal.
At Barends Psychology Practice, we treat Post-traumatic stress disorder Online and in person. Book your first, free of charge, session now. Go to contact us. (Depending on your health insurance, treatment may be reimbursed).
Jump-to:
- What is Post-traumatic stress disorder?
- PTSD symptoms.
- PTSD causes.
- PTSD diagnosis.
- PTSD treatment?
- Online EMDR treatment.
- How to cope with PTSD?
- PTSD facts.
- PTSD checklist.
- Take me to the homepage.
Partner with PTSD – understanding why your partner responds the way they do

During normal daily activities, someone with PTSD may respond out of character or out of proportion to the situation. For someone who is not traumatized it can be very difficult to understand why the other person responds so extreme. This extreme response can easily lead to a discussion or argument, and feelings of isolation and withdrawal in the partner with PTSD.
For someone with PTSD it is very difficult to respond in a different way, because they are being triggered by something that reminds them of the traumatic event. This reminder can be external (something someone else says or does; a certain location or person) or internal (a memory, familiar smell, sound, feeling, taste) and is, of course, very personal. Each reminder of the traumatic response can trigger PTSD symptoms such as heart palpitations, trembling, flashbacks, mood swings, dissociation, and more.
We’ve created an image (“How does someone get triggered”) with different examples to illustrate how a normal event can trigger PTSD symptoms in someone with PTSD. In this image each example triggers a different traumatic event.
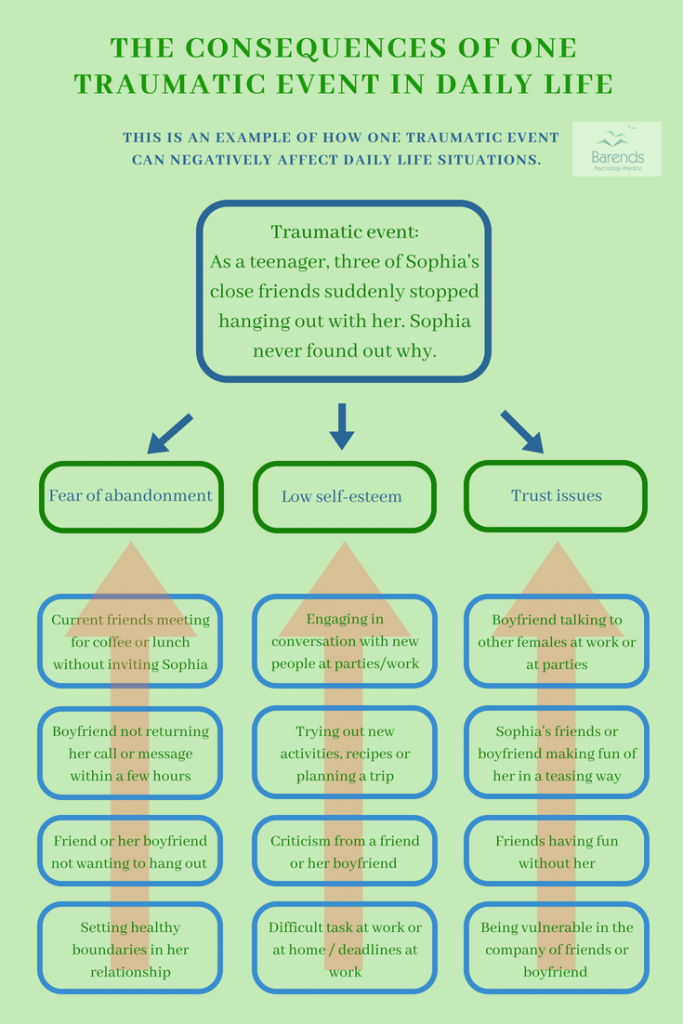
However, one traumatic event could also be triggered in multiple ways, as can be seen in the other image (“The consequences of one traumatic event in daily life”). In this image the traumatic event created a fear of abandonment, trust issues, and low self-esteem. The examples trigger one of these issues and negatively affect Sophia’s life. For instance, Sophia reaches out more to her friends/partner if they do not respond within a few hours after she sent them a message. Sophia is afraid that her friends/partner will abandon her. Her friends/partner may feel pressured to respond as soon as possible and/or may start to take some distance from Sophia, because she is too needy.
(Advertisement. For more information, continue reading).
Another example: If her partner criticizes her for setting boundaries (a combination of two examples), she may feel like her partner will abandon her and she may feel like she is not ‘good enough of a partner’ – notice the parallel with the traumatic event. As a consequence, she may stop setting boundaries to avoid criticism.
Often, people with PTSD are not aware of their own triggers and cannot explain why they respond the way they do. This can add to the frustration of the partner.
Partner with PTSD – tips and advice
Create a list with triggers:
A list with PTSD triggers makes it easier to predict how your partner will respond in certain situation, and also what to avoid. For instance, avoiding war movies if it triggers a war veteran with PTSD or returning calls immediately if your partner got rejected/abandoned by friends. Writing down how your partner with PTSD will respond in certain situations will help the both of you even more.
Being supportive:
Supporting your partner whenever they feel down or sad helps them to get through that difficult moment. Although your partner with PTSD may have a lot of negative thoughts and feelings, it is important to stay positive. Avoid negative reactions (disregarding their feelings or telling them to move on, for instance) as they can increase PTSD symptoms [2] just like negative religious coping: feeling punished by God for one’s sins or lack of spirituality [3]. Negative religious coping makes people with PTSD feel worse and does not reduce their PTSD symptoms.
Here are items one can think of when offering social support. In which way do you offer social support to your partner with PTSD? Take the poll and compare your results with the answers of others.
Prevent avoidant coping:
Avoidant coping may work in the short run, but increases PTSD symptoms in the long run [4],[5],[6]. Although internal and external reminders of the traumatic event are painful and everything but fun, remember that they are temporary and will disappear in time. It is important to help your partner to stop avoiding internal and external reminders of PTSD for at least a little while each day. For more information about internal and external reminders, go to: coping with PTSD. Don’t force your partner to face the flashbacks, memories, thoughts, and feelings all the time, especially not if they have them a lot. In that case we recommend PTSD treatment and in the mean while offering a little distraction.
(Advertisement. For more information about PTSD, continue reading).
Motivate them:
Motivate your partner to stick to a healthy rhythm and to reach out to friends and family for social support. A healthy rhythm is important for your partner with PTSD, because it reduces sleeping problems and nightmares. A healthy rhythm increases the chances for them to be in time for work and to be in time for appointments.
The more friends and relatives your partner can turn to for support, the better. You do not have to be her only support; it may not be enough and you may not be able to give all your partner needs. Every person has a slightly different take on situations and gives different advice. On top of that you can recharge yourself a little bit in the mean time as well.
Cognitive appraisal:
In general, people with PTSD have a more negative view on life; they more often than others have a negative mood and struggle to get through the day. It is no surprise that they label certain tasks as problems instead of challenges. Labeling tasks in terms of problems is associated with more negative emotions, more feelings of hopelessness and stress [7].
Cognitive appraisal basically means to label a task differently, in a more positive way. Labeling tasks in terms of challenges is associated with low negative emotions, positive arousal, and feelings of being in control [7],[8]. Helping your partner with PTSD to re-evaluate certain tasks will improve their mood, especially when they ‘win a challenge’.
Literature
- [1] Karney, B. R., Ramchand, R., Osilla, K. C., Caldarone, L. B., & Burns, R. M. (2008). Predicting the immediate and long-term consequences of post-traumatic stress disorder, depression, and traumatic brain injury in veterans of Operation Enduring Freedom and Operation Iraqi Freedom. Invisible wounds of war, 119.
- [2] Ullman, S. E., Townsend, S. M., Filipas, H. H., & Starzynski, L. L. (2007). Structural models of the relations of assault severity, social support, avoidance coping, self-blame, and PTSD among sexual assault survivors. Psychology of Women Quarterly, 31, 23-37.
- [3] Feder, A., Ahmad, S., Lee, E. J., Morgan, J. E., Singh, R., Smith, B. W., … & Charney, D. S. (2013). Coping and PTSD symptoms in Pakistani earthquake survivors: Purpose in life, religious coping and social support. Journal of affective disorders, 147, 156-163.
- [4] Lawrence, J. W., & Fauerbach, J. A. (2003). Personality, coping, chronic stress, social support and PTSD symptoms among adult burn survivors: a path analysis. The Journal of burn care & rehabilitation, 24, 63-72.
- [5] Iverson, K. M., Litwack, S. D., Pineles, S. L., Suvak, M. K., Vaughn, R. A., & Resick, P. A. (2013). Predictors of intimate partner violence revictimization: The relative impact of distinct PTSD symptoms, dissociation, and coping strategies. Journal of traumatic stress, 26, 102-110.
- [6] Pineles, S. L., Mostoufi, S. M., Ready, C. B., Street, A. E., Griffin, M. G., & Resick, P. A. (2011). Trauma reactivity, avoidant coping, and PTSD symptoms: A moderating relationship? Journal of abnormal psychology, 120, 240.
- [7] Olff, M., Langeland, W., & Gersons, B. P. (2005). The psychobiology of PTSD: coping with trauma. Psychoneuroendocrinology, 30, 974-982.
- [8] Prati, G., & Pietrantoni, L. (2009). Optimism, social support, and coping strategies as factors contributing to posttraumatic growth: A meta-analysis. Journal of loss and trauma, 14, 364-388.