 What is bipolar disorder?
What is bipolar disorder?
People with bipolar disorder experience typical bipolar disorder symptoms such as: heavy mood swings, huge changes in energy level, activity level, and experience difficulty carrying out daily tasks. Mood shifts occur in a range of a few times a day to a few times a year. The severity and/or disruptive nature of the bipolar disorder symptoms make it difficult for people with bipolar disorder to maintain healthy relationship or keep jobs for longer periods of time. Also, people with bipolar disorder are at more risk of developing dementia [20], obesity and metabolic syndrome [21]. People with bipolar disorder are more likely to commit suicide, almost always during a depressive episode [17].
Fortunately, bipolar disorder is treatable and with the right type of counseling, the severity of the symptoms can be reduced and a healthy and normal life can be maintained.
This page covers the following topics: explanation of bipolar disorder, bipolar disorder symptoms, bipolar disorder risk factors, and facts.
Quick Jump-to menu:
- Bipolar causes, treatment, and diagnosis.
- Bipolar disorder self-help and partner-help (coming soon).
- Bipolar disorder online test (coming soon).
- Online treatment for bipolar disorders.
- Back to the homepage.
At Barends Psychology Practice, we offer counseling for bipolar disorder. Schedule a first, free of charge, session now, go to: contact us. (Depending on your health insurance, treatment may be reimbursed).
Bipolar disorder terminology.
Mania – The elevated mood is called a mania, or hypomania (depending on the severity). The bipolar disorder symptoms during mania make people feel euphoric, full of energy, and sometimes irritable. They are impulsive in their decisions (they don’t think of the consequences) and sleep little.
Depression – The bipolar disorder symptoms during periods of depression are characterized by feelings of sadness, anxiety, guilt, hopelessness, and isolation. People often loss interest in activities they like, report changes in sleep and appetite, loneliness, and feel indifferent.
Mixed affective episodes – During such episodes people experience Mania and Depression at the same time. During such periods there is an increased risk of suicide, because depressive emotions are often accompanied by impulsiveness.
(Advertisement. For more information, continue reading.)
Bipolar types: I, II and cyclothymia.
There are four main types of Bipolar disorder (BD): type I, type II, cyclothymia, and Not Otherwise Specified.
Bipolar Type I is characterized by at least one full-blown manic episode lasting at least one week. The bipolar disorder symptoms are severe enough to disrupt the patients ability to work and function socialize. Hospitalisation sometimes in required to prevent harm to themselves or others.
Bipolar Type II is less severe than type I. Although you can have an elevated mood and changes in your functioning, you are able to carry out daily tasks. People with type II experience longer depressive episodes than manic episodes.
Cyclothymia is a less severe type of bipolar disorder than Type I and Type II. Cyclothymia is characterised by short manic and depressive episodes (too short to meet the criteria for major affective syndromes like bipolar disorder or major depressive disorder.
Bipolar disorder Not Otherwise Specified is a category of bipolar disorders that do not fit into the above mentioned categories: drug-induced bipolar disorder and bipolar disorder caused by a medical condition.
Bipolar disorder symptoms.
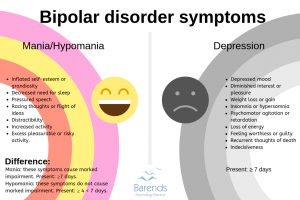 The manic, hypomanic, and depressive episodes contain contradicting bipolar disorder symptoms which can be quite confusing. Someone who experiences a depressive episode, for example, may lack energy, prefers sleeping throughout the day, and may not enjoy most of the daily activities. Someone who experiences a manic episode, however, may feel energetic, happy, and does not need to sleep (much) at all.
The manic, hypomanic, and depressive episodes contain contradicting bipolar disorder symptoms which can be quite confusing. Someone who experiences a depressive episode, for example, may lack energy, prefers sleeping throughout the day, and may not enjoy most of the daily activities. Someone who experiences a manic episode, however, may feel energetic, happy, and does not need to sleep (much) at all.
For some people it is easier to look at the symptoms per episode to determine whether it was a depressive, manic or hypomanic episode. Therefore, we’ve created an overview of the symptoms categorised according to episodes.
Depressive episode:
There are 3 criteria to keep in mind:
- the symptoms must be present nearly every day,
- they must cause functional impairment, and
- they cannot be better explained by other mental disorders, drugs misuse, or medication side-effects.
- Depressive mood most of the day,
- Marked weight loss (while not dieting) or weight gain,
- Diminished interest or pleasure,
- Insomnia or hypersomnia,
- Fatigue or loss of energy,
- Psychomotor agitation or retardation,
- Diminished ability to concentrate or think, or being indecisive,
- Recurrent thoughts of death and/or suicidal ideations,
- Inappropriate or excessive guilt or feelings of worthlessness.
Manic episode:
There are 3 criteria to keep in mind:
- the symptoms must be present nearly every day and most of the day,
- the symptoms must be present for one week or longer, and
- they cannot be better explained by other mental disorders, drugs misuse, or medication side-effects.
- Inflated self-esteem or grandiosity,
- Pressured speech,
- Decreased need for sleep,
- Racing thoughts or flight of ideas,
- Distractability,
- Increased activity,
- Excess pleasurable or risky activities,
Hypomanic episode:There are 4 criteria to keep in mind:
- the symptoms must be present nearly every day and most of the day,
- the symptoms must be present between four and six days,
- are not severe enough to cause marked impairment, and
- cannot be better explained by other mental disorders, drugs misuse, or medication side-effects.
- Inflated self-esteem or grandiosity,
- Pressured speech,
- Decreased need for sleep,
- Racing thoughts or flight of ideas,
- Distractability,
- Increased activity,
- Excess pleasurable or risky activities,
Bipolar disorder risk factors
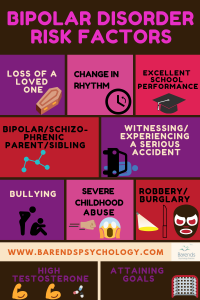 There are several factors that may contribute to the development of Bipolar disorder or the bipolar disorder symptoms. Fortunately, not every risk factor leads to the development of bipolar disorder or one of its symptoms. A risk factor simply means that the chance of developing something increases when someone meet that criterion.
There are several factors that may contribute to the development of Bipolar disorder or the bipolar disorder symptoms. Fortunately, not every risk factor leads to the development of bipolar disorder or one of its symptoms. A risk factor simply means that the chance of developing something increases when someone meet that criterion.
Genetics:
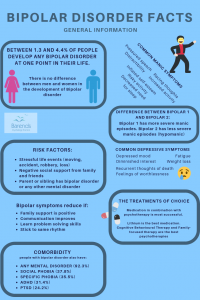
Having a parent or sibling with schizophrenia or bipolar disorder also increases the chance of developing bipolar disorder [19]. With a heritability of 59%, there is a strong genetic risk factor of developing bipolar disorder [19]. Interestingly, being a man or female does not increase or decrease the chance of developing bipolar disorder [19].
Stressful life events:
Experiencing a stressful life event, such as moving away, losing a significant person, an accident, robbery or being bullied increases the chance of developing bipolar disorder [9]. If someone loses his mom before the age of 5, for instance, there is a significantly increased chance of developing bipolar disorder and even at an earlier age [10]. Losing a mother can have a huge impact on the emotional development of a child.
Psychosocial:
A change in social rhythm or circadian rhythm increases the chance of developing a bipolar disorder episode [9]. This suggests that sticking to a healthy day and night rhythm is very important for people with bipolar disorder.
Receiving negative social support from close ones also increases the risk of experiencing a bipolar disorder episode and can worsen the bipolar disorder symptoms during an episode [9]. Examples of negative social support are a guilt-inducing, critical, and intrusive statements. Staying calm when a close one experiences a depressive or manic episode can be quite challenging.
One of the most interesting facts may be that individuals with excellent school performance are 4 times as likely to develop bipolar disorder compared to those who perform average or below average. At the same time, people with the poorest grades were also moderately more at risk of developing bipolar disorder [22]
(Advertisement. For more Bipolar disorder facts, continue reading).
Bipolar disorder facts
We’ve gathered interesting bipolar disorder facts from around the world and categorized them in different categories. Did you know that BD is not related to sex, family income or race/ethnicity [1],[6] or that people with BD have more bed-rest days due to emotional problems compared to people with other mental disorders [3]? Interestingly, one of the Bipolar disorder facts states that BD is responsible for more disability-adjusted life-years than cancer, epilepsy, and Alzheimer disease [5]. Another one of the Bipolar disorder facts is that one in four people with BP-1 or Any Bipolar Disorder report a history of suicide attempts compared to one in five with BP-2 [5],[7].
At Barends Psychology Practice, we offer counseling for bipolar disorder. Schedule a first, free of charge, session now, contact us. (Depending on your health insurance, treatment may be reimbursed).
Bipolar disorder facts – Any bipolar disorder
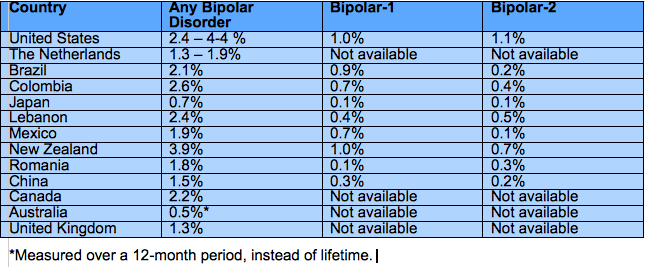
Between 0.7 and 4.4% of people experience any Bipolar disorder at one point in time [1],[2],[3],[4],[6],[8]. This includes: BD-1, BD-2, Cyclothymia, Substance-Induced BP, BP associated with another medical condition, and BD Not Otherwise Specified.
On average, in the United States, Bipolar disorders develop at the age of 20.8 years [1]. This is slightly later than the age of onset of Bipolar-1 and Bipolar-2. In Canada, however, the age of onset for Bipolar disorder is 22.5 years [6].
92.3% of the people with any Bipolar disorder meet the criteria for another mental disorder as well; for instance, one in every three people with Bipolar disorder also has social phobia (37.8%), ADHD (31.4%), one in every four people has PTSD, and one in every five people has Panic Disorder [1].
Bipolar disorder facts – Bipolar disorder 1
Between 0.4 and 1% of adults experiences Bipolar disorder 1 at one point in their life; 0.8% of men and 1.1% of women [1],[2]. Some countries report 0.1% of their population, but they used different criteria. Interestingly, some studies report no gender differences in people with bipolar disorder [19].
The age of onset for BP1 is 18.2 years: in retrospect people with BP-1 experienced either a manic/hypomanic or major depressive episode at 18.2 years [1].
People with BP-1 reported an average of 10.3 years in episode (manic/hypomanic/major depressive episode) [1].
Approximately one in three people (35.3%) with BP-1 received inappropriate medication in the past 12 months [1]. 46.8% received no medication at all [1].
97.7% of people with Bipolar-1 meets the criteria for another mental disorder as well; for instance, almost half of the people with Bipolar-1 also has social phobia (51.6%) or specific phobia (47.1%), one in every three people has Panic Disorder (29.1%), PTSD (30.9%), and one in every four people has OCD [1].
Bipolar disorder facts -Bipolar disorder 2
Between 0.1 and 1.1% of adults experiences Bipolar disorder 2 at one point in their life; 0.9% of men and 1.3% of women [1],[2]. Interestingly, some studies report no gender differences in people with bipolar disorder [19].
For Bipolar disorder 2, the age of onset is 20.3 years: in retrospect people with BP2 experienced either a manic/hypomanic or major depressive episode at 20.3 years [1].
On average, people with BP-2 are in episode for 11.6 years (manic/hypomanic/major depressive episode) [1].
One in four people (24.5%) with BP-2 received inappropriate medication in the past 12 months [1]. 59.9% received no medication at all [1].
95.8% of people with Bipolar-2 meets the criteria for another mental disorder as well; for instance, one in every two people with Bipolar-2 also has specific phobia (51.1%), social phobia (54.6%), one in three people has PTSD (34.3%), GAD (37.0%), one in four people has Panic Disorder (27.2%), and one in every five people has OCD (20.8%) [1].
Bipolar disorder facts – Risk factors
Prior to onset or subsequent episodes of Bipolar disorder, individuals often experience stressful life events [9]. A stressful life event increases the chance of developing a depressive episode as well as a manic/hypomanic episode. Stressful life events could be a renovation, moving to a different city/country, a serious accident, robbery, the loss of a significant other, and so on.
(Advertisement. For more Bipolar disorder facts, continue reading).
Research suggests that life events that disrupt the circadian rhythm or daily social rhythms more often predict mood episodes (depression, manic or hypomanic) compared to life events that do not disrupt the circadian or daily social rhythm [9]. During Ramadan, for instance, Muslims with BD more often experience an episode compared to the period outside Ramadan [9].
Goal striving or goal attainment is associated with experiencing manic/hypomanic episodes [9]. The theory behind these bipolar disorder facts is that people with BD respond with extreme positive effect, high energy, and motivation to events that involve high incentive motivations and goal striving. At the same time, people respond with extreme negative effect, anhedonia, and low energy to situations involving uncontrollable loss and failure [9].
Negative social support from family and friends predicts a worse course of bipolar disorder or the bipolar disorder symptoms. An example of negative social support: high expressed emotions [9].
Severe childhood abuse is a predictor of bipolar disorder later in life. Almost half of the people with bipolar disorder experienced severe childhood abuse [18]. People with bipolar disorder who were severely abused as a child also experienced their first episode earlier compared to those without a history of childhood abuse [18].
Positive social support from family and friends, on the other hand, can serve as a buffer against the deleterious effects of stress, and can enhance functioning among people with BD [9]. Positive social support can reduce the impact of some of the bipolar disorder symptoms
Problem solving skills, better communication, and psycho-education reduce the effects of BD and the chances of a relapse [9].
The chance of developing bipolar Disorder increases 13.63-fold when a sibling or parent has BD or another mental disorder [10].
Losing a mother before age 5 is also associated with increased chances (4.05-fold) of developing BD [10].
Research suggests that Bipolar disorder is a polygenic disease influenced by many genes that each contribute a little bit [11].
The suicide rate is 25 times higher for people with Bipolar disorder compared to the normal population [17]. Suicidal behaviour almost exclusively occurs during a depressive episode [17].
Higher testosterone levels are associated with more manic episodes and more suicide attempts [16].
Bipolar disorder facts – Treatment
Lithium has been the drug of choice for decades for the treatment of Bipolar disorder. Lithium is a mood stabilizer [12] and helps most of the bipolar disorder symptoms to reduce or disappear. Lithium and the anticonvulsant lamotrigine are the only two medications for which long-term efficacy has been established in at least two placebo-controlled studies [13].
During Lithium treatment the annual attempted suicide rate is 13-fold lower compared to the annual attempted suicide rate while not taking Lithium [13],[14].
Cognitive-behavioural therapy, family-focused therapy, interpersonal and social rhythm therapy, group psychoeducation, and systematic care management are all evidence-based treatments for Bipolar disorder [15].
Psychotherapy is most likely not effective during a manic episode, because of insufficient insight or rejection of help [15].
Bipolar disorder facts – Literature
[1] Merikangas, K. R., Akiskal, H. S., Angst, J., Greenberg, P. E., Hirschfeld, R. M., Petukhova, M., & Kessler, R. C. (2007). Lifetime and 12-month prevalence of bipolar spectrum disorder in the National Comorbidity Survey replication. Archives of general psychiatry, 64, 543-552.
[2] Merikangas, K. R., Jin, R., He, J. P., Kessler, R. C., Lee, S., Sampson, N. A., … & Ladea, M. (2011). Prevalence and correlates of bipolar spectrum disorder in the world mental health survey initiative. Archives of general psychiatry, 68, 241-251.
[3] ten Have, M., Vollebergh, W., Bijl, R., & Nolen, W. A. (2002). Bipolar disorder in the general population in The Netherlands (prevalence, consequences and care utilisation): results from The Netherlands Mental Health Survey and Incidence Study (NEMESIS). Journal of affective disorders, 68, 203-213.
[4] de Graaf, R., Ten Have, M., van Gool, C., & van Dorsselaer, S. (2012). Prevalence of mental disorders and trends from 1996 to 2009. Results from the Netherlands Mental Health Survey and Incidence Study-2. Social psychiatry and psychiatric epidemiology, 47, 203-213.
[5] World Health Organization, The World Health Report 2002: Reducing Risks, Promoting Healthy Life. Geneva, Switzerland World Health Organization, 2002.
[6] Schaffer, A., Cairney, J., Cheung, A., Veldhuizen, S., & Levitt, A. (2006). Community survey of bipolar disorder in Canada: lifetime prevalence and illness characteristics. The Canadian Journal of Psychiatry, 51, 9-16.
[7] Mitchell, P. B., Slade, T., & Andrews, G. (2004). Twelve-month prevalence and disability of DSM-IV bipolar disorder in an Australian general population survey. Psychological Medicine, 34, 777-785.
[8] Smith, D. J., Nicholl, B. I., Cullen, B., Martin, D., Ul-Haq, Z., Evans, J., … & Hotopf, M. (2013). Prevalence and characteristics of probable major depression and bipolar disorder within UK biobank: cross-sectional study of 172,751 participants. PloS one, 8, e75362.
[9] Alloy, L. B., Abramson, L. Y., Urosevic, S., Walshaw, P. D., Nusslock, R., & Neeren, A. M. (2005). The psychosocial context of bipolar disorder: environmental, cognitive, and developmental risk factors. Clinical psychology review, 25, 1043-1075.
[10] Mortensen, P. B., Pedersen, C. B., Melbye, M., Mors, O., & Ewald, H. (2003). Individual and familial risk factors for bipolar affective disorders in Denmark. Archives of general psychiatry, 60, 1209-1215.
[11] Baum, A. E., Akula, N., Cabanero, M., Cardona, I., Corona, W., Klemens, B., … & Georgi, A. (2008). A genome-wide association study implicates diacylglycerol kinase eta (DGKH) and several other genes in the etiology of bipolar disorder. Molecular psychiatry, 13, 197.
[12] Su, Y., Ryder, J., Li, B., Wu, X., Fox, N., Solenberg, P., … & Ni, B. (2004). Lithium, a common drug for bipolar disorder treatment, regulates amyloid-β precursor protein processing. Biochemistry, 43, 6899-6908.
[13] Goodwin, F. K., Fireman, B., Simon, G. E., Hunkeler, E. M., Lee, J., & Revicki, D. (2003). Suicide risk in bipolar disorder during treatment with lithium and divalproex. Jama, 290(11), 1467-1473.
[14] Baldessarini, R. J., Tondo, L., & Hennen, J. (2001). Treating the suicidal patient with bipolar disorder. Annals of the New York Academy of Sciences, 932, 24-43.
[15] Geddes, J. R., & Miklowitz, D. J. (2013). Treatment of bipolar disorder. The Lancet, 381, 1672-1682.
[16] Sher, L., Grunebaum, M. F., Sullivan, G. M., Burke, A. K., Cooper, T. B., Mann, J. J., & Oquendo, M. A. (2012). Testosterone levels in suicide attempters with bipolar disorder. Journal of psychiatric research, 46, 1267-1271.
[17] Rihmer, Z. (2009). Suicide and bipolar disorder. In Bipolar depression: molecular neurobiology, clinical diagnosis and pharmacotherapy (pp. 47-56). Birkhäuser Basel.
[18] Garno, J. L., Goldberg, J. F., Ramirez, P. M., & Ritzler, B. A. (2005). Impact of childhood abuse on the clinical course of bipolar disorder. The British Journal of Psychiatry, 186(2), 121-125.
[19] Lichtenstein, P., Yip, B. H., Björk, C., Pawitan, Y., Cannon, T. D., Sullivan, P. F., & Hultman, C. M. (2009). Common genetic determinants of schizophrenia and bipolar disorder in Swedish families: a population-based study. The Lancet, 373, 234-239.
[20] Kessing, L. V., & Andersen, P. K. (2004). Does the risk of developing dementia increase with the number of episodes in patients with depressive disorder and in patients with bipolar disorder?. Journal of Neurology, Neurosurgery & Psychiatry, 75, 1662-1666.
[21] Fiedorowicz, J. G., Palagummi, N. M., Forman-Hoffman, V. L., Miller, D. D., & Haynes, W. G. (2008). Elevated prevalence of obesity, metabolic syndrome, and cardiovascular risk factors in bipolar disorder. Annals of Clinical Psychiatry, 20, 131-137.
[22] MacCabe, J. H., Lambe, M. P., Cnattingius, S., Sham, P. C., David, A. S., Reichenberg, A., … & Hultman, C. M. (2010). Excellent school performance at age 16 and risk of adult bipolar disorder: national cohort study. The British Journal of Psychiatry, 196, 109-115.
