How to Help Your Partner with PTSD
Experiencing a traumatic event is more common than most people think. A car accident, being robbed, a natural disaster (hurricane, earthquake), losing a loved one, or being sexually assaulted are all examples of traumatic events. Other examples include being bullied, moving to another city or country, and being fired. In response to these traumatic events, it is normal to experience some post-traumatic stress disorder (PTSD) symptoms. Sleeping problems, mood swings, flashbacks, and difficulty concentrating are common PTSD symptoms. Additionally, PTSD can negatively affect social and occupational functioning [1].
For most people, these symptoms fade within weeks after the traumatic event. However, for some, the symptoms persist and develop into PTSD. Living with PTSD often means dealing with chronic sleeping problems, nightmares, and difficulty concentrating. At any moment, someone with PTSD can be triggered or experience a flashback. These flashbacks and triggers are accompanied by feelings of anxiety, terror, panic, sadness, or anger. PTSD does not resolve on its own, and avoiding triggers can lead to increased suffering in the long run.
Recommendation
For those struggling with PTSD, we recommend reading the following self-help page for tips and coping strategies: Coping with PTSD. If your partner has PTSD, we strongly encourage you to read this page to better understand the symptoms they may experience and how you can support them.
Having a partner with PTSD can be challenging because their responses may be unpredictable, out of character, or disproportionate to the situation. They may treat you unfairly or come across as uninterested, unloving, or emotionally distant. However, it is important to remember that this behavior is not personal.
At Barends Psychology Practice, we treat Post-traumatic stress disorder. Book your first, free session now. Go to contact us.
Jump-to:
- What is Post-traumatic stress disorder?
- PTSD symptoms.
- PTSD causes.
- PTSD diagnosis.
- Workplace PTSD.
- PTSD treatment?
- Online EMDR treatment.
- How to cope with PTSD?
- PTSD facts.
- PTSD test.
- Take me to the homepage.
Partner with PTSD – Understanding Why Your Partner Responds the Way They Do
During daily activities, someone with PTSD may react in ways that seem out of character or disproportionate to the situation. For someone who has not experienced trauma, it can be difficult to understand why their partner responds so intensely. These extreme reactions can easily lead to arguments, feelings of isolation, and emotional withdrawal in the partner with PTSD.
For individuals with PTSD, changing their response is challenging because they are being triggered by something that reminds them of the traumatic event. These triggers can be external (such as something someone says or does, a specific location, or a particular person) or internal (such as a memory, familiar smell, sound, feeling, or taste). Triggers are highly personal, and each one can evoke PTSD symptoms, including heart palpitations, trembling, flashbacks, mood swings, dissociation, and more.
To illustrate how everyday situations can trigger PTSD symptoms, we have created an image titled “How Does Someone Get Triggered?” This image provides examples of how seemingly normal events can act as triggers for someone with PTSD, with each scenario linked to a different traumatic experience.
Example
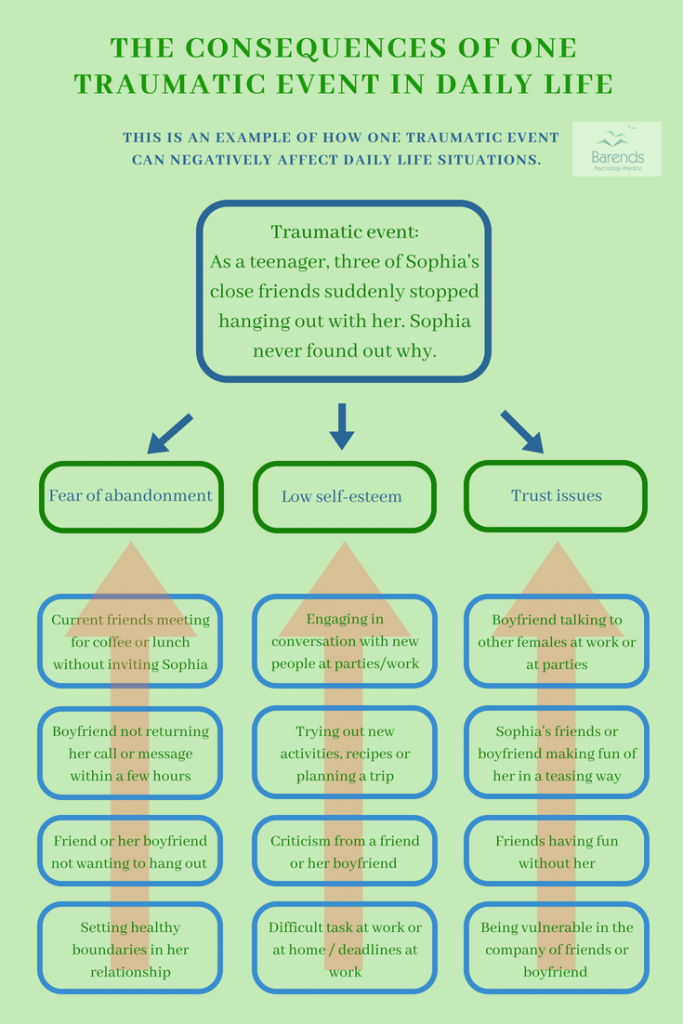
However, a single traumatic event can also be triggered in multiple ways, as demonstrated in another image: “The Consequences of One Traumatic Event in Daily Life.” This image highlights how a traumatic experience can lead to issues such as fear of abandonment, trust issues, and low self-esteem. The examples show how these underlying fears can impact Sophia’s life.
For instance, if Sophia’s friends or partner do not respond to her messages within a few hours, she may reach out repeatedly, fearing abandonment. As a result, her friends or partner may feel pressured to reply quickly or may start distancing themselves because they perceive her as overly needy.
(Advertisement. For more information, continue reading).
Another example: If her partner criticizes her for setting boundaries (a combination of two triggers), she may feel as though she is not “a good enough partner” and fear abandonment—mirroring her original traumatic experience. Consequently, she may stop setting boundaries to avoid further criticism.
Many people with PTSD are unaware of their own triggers and cannot always explain why they react the way they do. This lack of awareness can add to the frustration of their partner, making communication and understanding even more challenging.
Partner with PTSD – Tips and Advice
Create a List of Triggers
Having a list of PTSD triggers makes it easier to anticipate how your partner may respond in certain situations and to identify what should be avoided. For example, if your partner is a war veteran with PTSD, avoiding war movies may be helpful. Similarly, if your partner has a history of rejection or abandonment by friends, promptly returning their calls can provide reassurance. Writing down how your partner typically reacts in certain situations can be beneficial for both of you.
Being Supportive
Supporting your partner during moments of sadness or distress can help them navigate difficult emotions. While your partner with PTSD may struggle with negative thoughts and feelings, it is important to remain positive. Avoid negative reactions—such as dismissing their feelings or telling them to “move on”—as these responses can worsen PTSD symptoms [2]. Similarly, negative religious coping, such as feeling punished by God for one’s sins or experiencing a lack of spirituality, can intensify distress rather than alleviate symptoms [3].
Here are some aspects to consider when offering social support. How do you support your partner with PTSD? Take the poll and compare your answers with those of others.
Preventing Avoidant Coping
Avoidant coping may provide temporary relief, but in the long run, it can exacerbate PTSD symptoms [4],[5],[6]. Although both internal and external reminders of the traumatic event can be painful and distressing, it is important to remember that they are temporary and will fade over time. Encourage your partner to gradually stop avoiding these reminders—at least for a short period each day.
For more information on internal and external reminders, visit: Coping With PTSD. However, do not pressure your partner to confront flashbacks, memories, or distressing thoughts and feelings constantly, especially if they experience them frequently. In such cases, PTSD treatment is recommended, and in the meantime, offering small distractions can be helpful.
(Advertisement. For more information about PTSD, continue reading).
Motivating Them
Encourage your partner to maintain a healthy daily routine and to reach out to friends and family for social support. A structured routine can reduce sleep disturbances and nightmares while improving punctuality for work and appointments.
The more sources of support your partner has, the better. You do not have to be their sole source of support—this may not be sufficient, and you may not be able to meet all of their emotional needs. Having multiple people to turn to provides a variety of perspectives and advice, and it also allows you to recharge when needed.
Cognitive Appraisal:
People with PTSD often have a more negative outlook on life, experiencing frequent low moods and difficulty managing daily tasks. As a result, they may perceive challenges as overwhelming problems rather than manageable tasks. Labeling tasks as “problems” is associated with increased negative emotions, stress, and feelings of hopelessness [7].
Cognitive appraisal involves reframing tasks in a more positive way. When tasks are seen as “challenges” rather than “problems,” they are associated with lower negative emotions, positive arousal, and a greater sense of control [7],[8]. Helping your partner reframe their perspective can improve their mood—especially when they successfully complete a challenge.
Literature
- [1] Karney, B. R., Ramchand, R., Osilla, K. C., Caldarone, L. B., & Burns, R. M. (2008). Predicting the immediate and long-term consequences of post-traumatic stress disorder, depression, and traumatic brain injury in veterans of Operation Enduring Freedom and Operation Iraqi Freedom. Invisible wounds of war, 119.
- [2] Ullman, S. E., Townsend, S. M., Filipas, H. H., & Starzynski, L. L. (2007). Structural models of the relations of assault severity, social support, avoidance coping, self-blame, and PTSD among sexual assault survivors. Psychology of Women Quarterly, 31, 23-37.
- [3] Feder, A., Ahmad, S., Lee, E. J., Morgan, J. E., Singh, R., Smith, B. W., … & Charney, D. S. (2013). Coping and PTSD symptoms in Pakistani earthquake survivors: Purpose in life, religious coping and social support. Journal of affective disorders, 147, 156-163.
- [4] Lawrence, J. W., & Fauerbach, J. A. (2003). Personality, coping, chronic stress, social support and PTSD symptoms among adult burn survivors: a path analysis. The Journal of burn care & rehabilitation, 24, 63-72.
- [5] Iverson, K. M., Litwack, S. D., Pineles, S. L., Suvak, M. K., Vaughn, R. A., & Resick, P. A. (2013). Predictors of intimate partner violence revictimization: The relative impact of distinct PTSD symptoms, dissociation, and coping strategies. Journal of traumatic stress, 26, 102-110.
- [6] Pineles, S. L., Mostoufi, S. M., Ready, C. B., Street, A. E., Griffin, M. G., & Resick, P. A. (2011). Trauma reactivity, avoidant coping, and PTSD symptoms: A moderating relationship? Journal of abnormal psychology, 120, 240.
- [7] Olff, M., Langeland, W., & Gersons, B. P. (2005). The psychobiology of PTSD: coping with trauma. Psychoneuroendocrinology, 30, 974-982.
- [8] Prati, G., & Pietrantoni, L. (2009). Optimism, social support, and coping strategies as factors contributing to posttraumatic growth: A meta-analysis. Journal of loss and trauma, 14, 364-388.