PTSD diagnosis
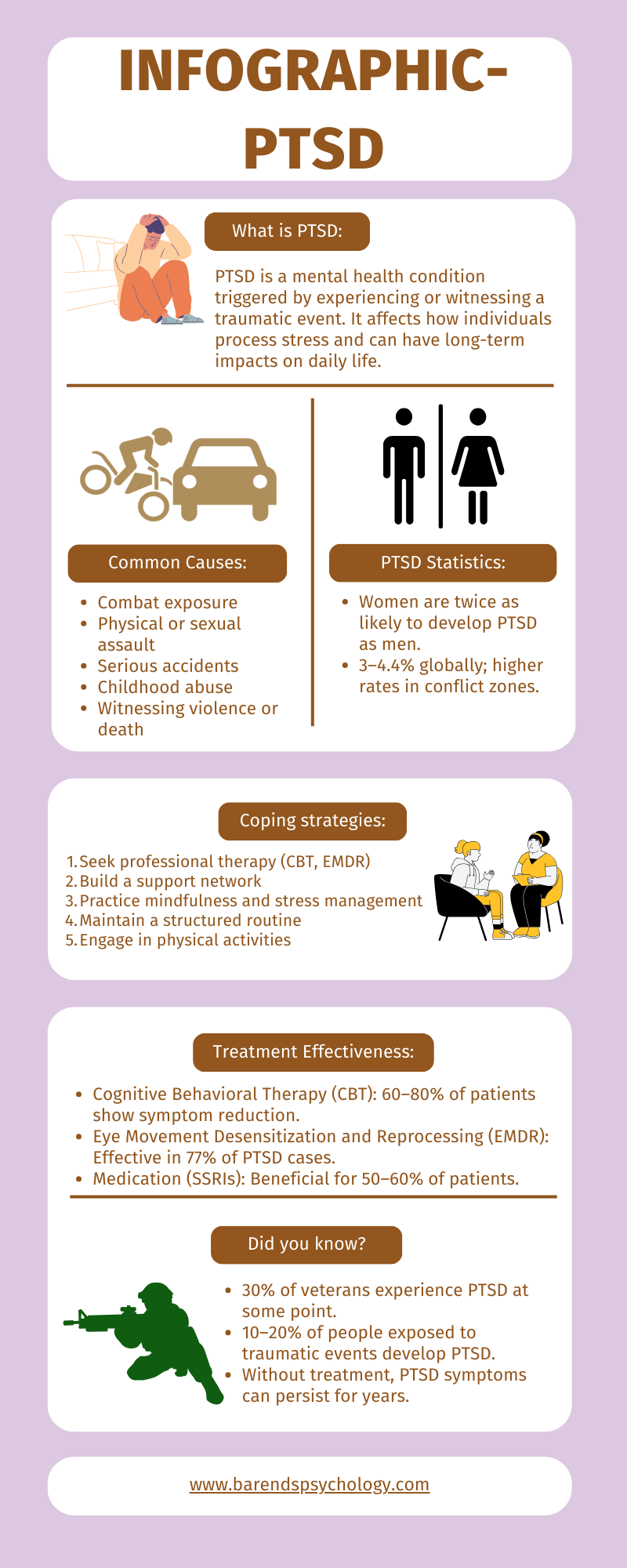
Post-traumatic stress disorder (PTSD) is a mental disorder that can develop after someone experiences a stressful or life-threatening event. Reacting with distress after experiencing trauma is a normal response of the body and brain. If this reaction lasts between 3 and 30 days, it is called Acute Stress Disorder (ASD) [1], or sometimes post-traumatic stress (PTS). In most people, these symptoms of PTSD disappear within four weeks after the traumatic event. However, in some individuals, PTSD symptoms persist, worsen, and negatively affect daily functioning. If someone continues to experience multiple PTSD symptoms after one month, a PTSD diagnosis may be given [1].
Compared to the outdated PTSD criteria (DSM IV), the DSM-5 diagnosis is more specific and accurate. For instance, a person’s reaction no longer needs to involve intense fear, helplessness, or horror, as such reactions do not significantly improve the diagnosis of PTSD. The updated criteria also clarify how PTSD develops: through direct exposure, witnessing the trauma, learning that a close friend or relative experienced trauma, or direct exposure to aversive details of traumatic events [2].
This page outlines the DSM-5 criteria for PTSD diagnosis and provides detailed explanations of specific criteria.
NOTE: The criteria below are sourced from the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), 2013 [2].
At Barends Psychology Practice, we treat Post-traumatic stress disorder Online and in person. Book your first, free session now. Go to Contact us.
Jump-to menu:
- What is Post-traumatic stress disorder?
- Post-traumatic stress disorder symptoms.
- Causes of PTSD.
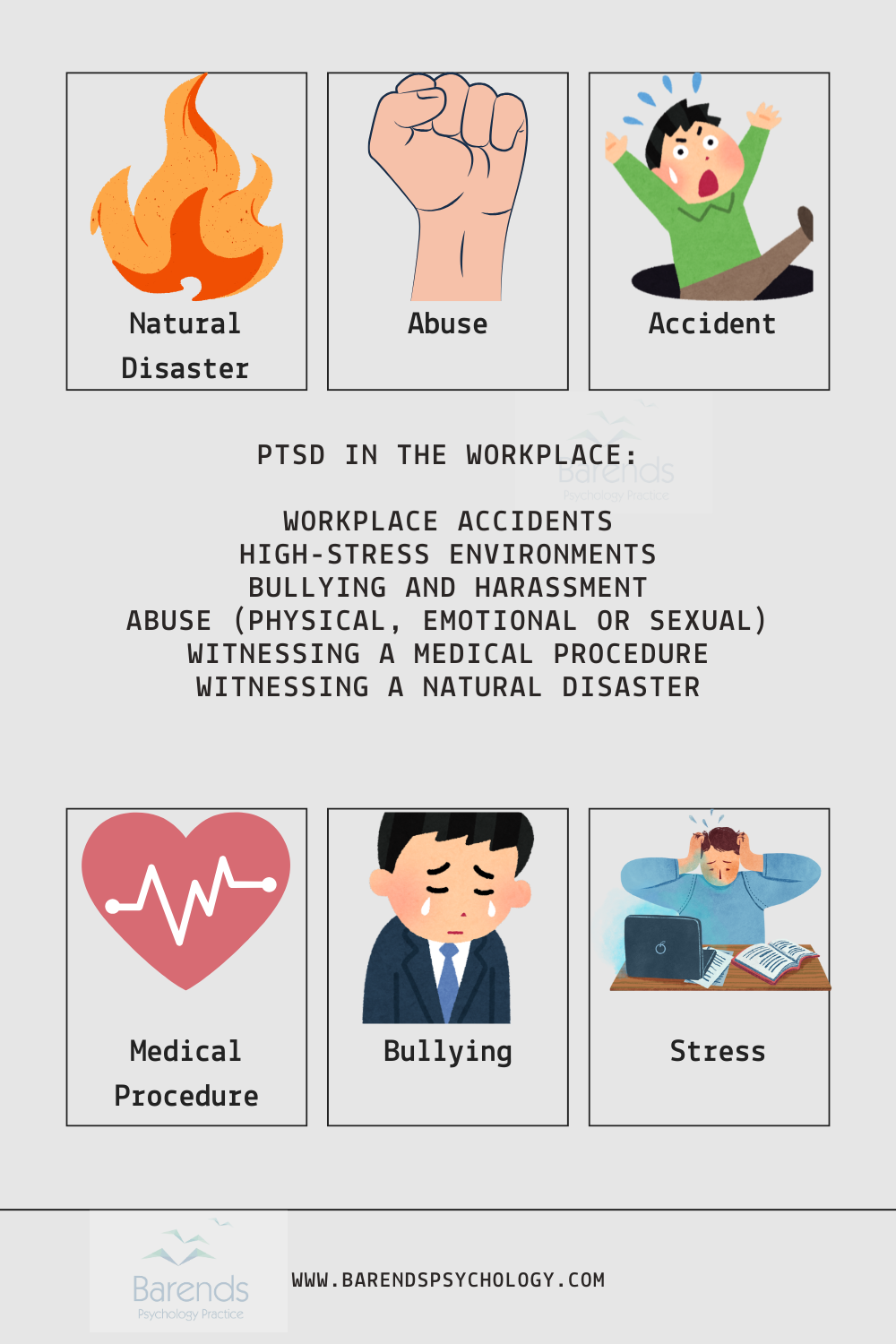
- Workplace PTSD.
- What are the post-traumatic stress disorder treatments?
- What is online PTSD treatment?
- How to cope with PTSD?
- Partner with PTSD.
- PTSD questionnaire.
- Interesting PTSD facts.
- Information about online counseling.
- Take me to the homepage.
PTSD Diagnosis – Criterion A: Trauma Exposure
This criterion establishes whether someone has experienced, witnessed, or learned about a traumatic event. It helps professionals and individuals understand the nature of the trauma.
Official DSM-5 Criterion:
The person was exposed to:
- death or threatened death,
- actual or threatened serious injury,
- actual or threatened sexual violence,
- Direct exposure (e.g., being involved in a serious car accident, surviving a natural disaster, experiencing an assault).
- Witnessing the trauma, in person (e.g., seeing a violent crime occur, witnessing a fatal accident).
- Indirectly, by learning that a close relative or close friend was exposed to trauma (e.g., finding out a family member was murdered or severely injured in an attack).
- Repeated or extreme indirect exposure to aversive details of the event(s) (e.g., first responders collecting body parts, therapists repeatedly hearing detailed accounts of child abuse).
PTSD Diagnosis – Criterion B: Intrusion Symptoms
This criterion focuses on how the traumatic event is persistently re-experienced.
Official DSM-5 Criterion:
The traumatic event is persistently re-experienced in the following way(s): (Only one symptom is required to meet this PTSD diagnosis criterion.)
- Intrusive thoughts. Recurrent, involuntary, and distressing memories of the trauma. Example: A survivor of a violent mugging may constantly recall the attack, struggling to focus on daily tasks.
- Nightmares. Disturbing dreams related to the trauma. Example: A car accident survivor may have frequent nightmares of crashing or being trapped in a vehicle.
- Dissociative reactions (e.g., flashbacks). The person may feel or act as if the traumatic event is happening again. Example: A combat veteran hearing fireworks might suddenly feel as if they are back in a war zone.
- Intense or prolonged distress after exposure to traumatic reminders. Example: A sexual assault survivor may experience extreme anxiety when seeing someone who resembles their attacker.
- Marked physiologic reactivity after exposure to trauma-related stimuli. Example: A person who survived a house fire may sweat profusely and experience a racing heart when smelling smoke.
PTSD Diagnosis – Criterion C: Avoidance
Many individuals with PTSD actively avoid trauma-related reminders to reduce distress.
Official DSM-5 Criterion:
Avoidance of trauma-related stimuli after the trauma, in the following way(s): (Only one symptom is required to meet this PTSD diagnosis criterion.)
- Avoiding trauma-related thoughts or feelings. Example: A robbery survivor refuses to think about the event or discuss it with anyone.
- Avoiding trauma-related external reminders (e.g., people, places, conversations, activities, objects, or situations). Example: A survivor of a school shooting avoids visiting the school or watching news about similar events.
PTSD Diagnosis – Criterion D: Negative Alterations in Cognition and Mood
PTSD affects emotions, thoughts, and beliefs about oneself and the world.
Official DSM-5 Criterion:
Negative thoughts or feelings that began or worsened after the trauma, in the following way(s): (Two symptoms are required to meet this PTSD diagnosis criterion.)
- Inability to recall key features of the trauma (not due to head injury, alcohol, or drugs). Example: A sexual assault survivor may forget specific details of the attack.
- Overly (and often distorted) negative thoughts and assumptions about oneself or the world. Example: A survivor of domestic violence might believe “I am unworthy of love.”
- Exaggerated blame of self or others for the trauma. Example: A car crash survivor blames themselves for the accident, even if they were not at fault.
- Negative emotions (e.g., fear, horror, anger, guilt, or shame).
- Decreased interest in pre-trauma activities. Example: A formerly outgoing person withdraws from social gatherings after experiencing an attack.
- Feeling isolated. Example: A war veteran feels disconnected from family and friends.
- Difficulty experiencing positive emotions. Example: A trauma survivor struggles to feel happiness or love.
(Advertisement. Scroll down for more information.)
PTSD Diagnosis – Criterion E: Alterations in Arousal and Reactivity
A traumatic event can cause heightened alertness and changes in behavior.
Official DSM-5 Criterion:
Trauma-related alterations in arousal and reactivity that began or worsened after the trauma, in the following way(s): (Two symptoms are required.)
- Irritability or aggression. Example: A person who survived a violent attack may become easily angered and aggressive.
- Risky or destructive behavior. Example: Engaging in reckless driving or substance abuse after a traumatic event.
- Hypervigilance. Example: Constantly scanning the environment for threats.
- Heightened startle reaction. Example: Jumping excessively at loud noises.
- Difficulty concentrating.
- Difficulty sleeping. Example: Insomnia due to frequent nightmares.
PTSD Diagnosis – Criterion F: Duration
Most people who experience a traumatic event recognize at least some of the above mentioned symptoms in the first few days after the traumatic event. Fortunately for most people, the majority of these symptoms disappear within a month after the traumatic event. If, however, these symptoms are still present after 1 month, then the PTSD diagnosis can be made.
Official DSM-5 Criterion:
- Symptoms last for more than 1 month.
PTSD Diagnosis – Criterion G: Functional Significance
Official DSM-5 Criterion:
- Symptoms create distress or functional impairment (e.g., social, occupational).
PTSD Diagnosis – Exclusion
Official DSM-5 Criterion:
- Symptoms are not due to medication, substance use, or other illness.
PTSD Diagnosis – Specifiers
Some individuals experience additional symptoms:
With Dissociative Symptoms:
- Depersonalization: Feeling detached from oneself.
- Derealization: Feeling that the world is unreal.
With Delayed Expression:
- Full PTSD diagnosis is not met until at least six months after the trauma.
Literature
- [1] Elklit, A., & Christiansen, D. M. (2010). ASD and PTSD in rape victims. Journal of Interpersonal Violence, 25, 1470-1488.
- [2] American Psychiatric Association. (2013) Diagnostic and statistical manual of mental disorders, (5th ed.). Washington, DC: Author.