Introduction to Borderline personality disorder symptoms
Definition:Borderline Personality Disorder (BPD) is defined in the DSM‑5‑Text Revision (DSM‑5‑TR) as a pervasive pattern of instability in interpersonal relationships, self-image, affect, and marked impulsivity. These Borderline Personality Disorder symptoms begin by early adulthood and occur across various contexts.
In the ICD‑11, BPD isn’t a standalone category but is represented via a Borderline Pattern specifier attached to ratings of personality disorder severity (mild/moderate/severe) alongside personality trait domain qualifiers.
Why the comparison matters:
DSM‑5‑TR retains a categorical approach (BPD as its own diagnosis), while ICD‑11 embraces a dimensional model (overall personality dysfunction with BPD characteristics as a qualifier). Both systems use overlapping criteria, but ICD‑11 adds a nuanced severity and trait-based framework: aligning more with modern clinical utility.
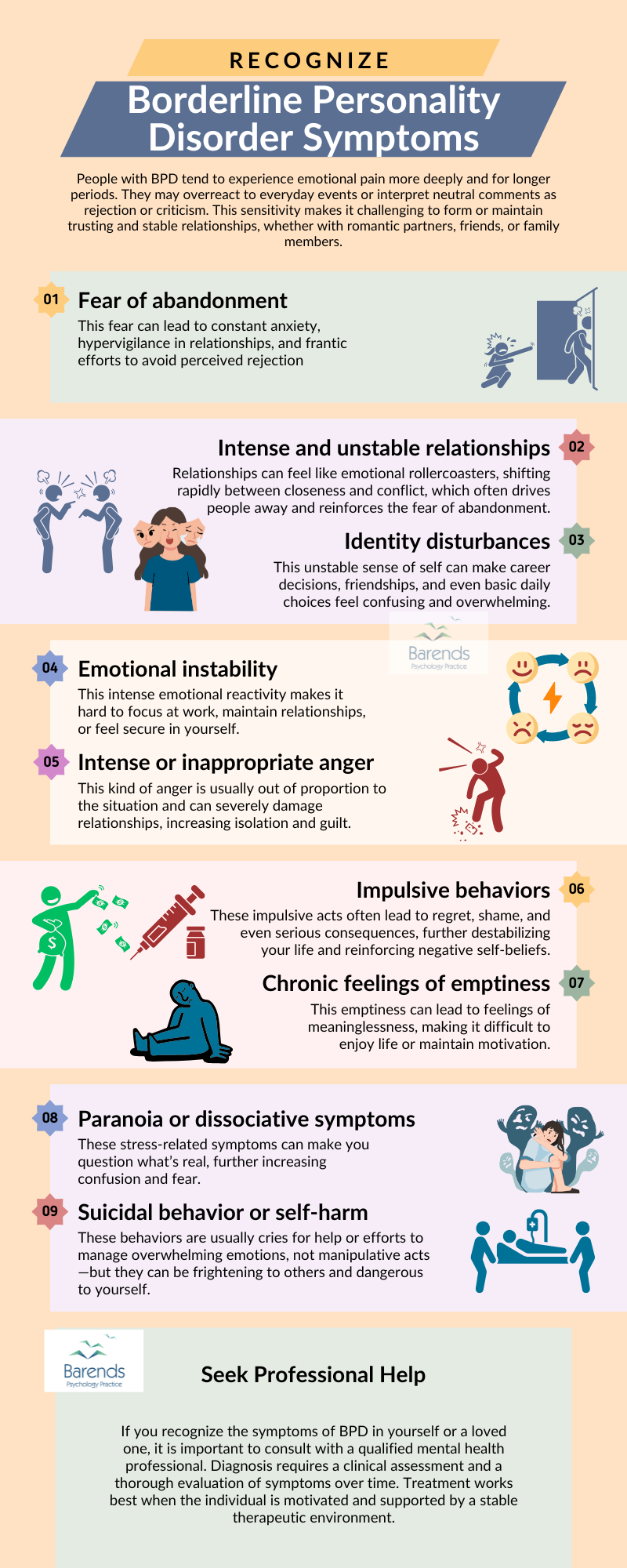
Borderline Personality Disorder Symptoms Explained
DSM‑5‑TR Criteria for BPD (9 Criteria)
DSM‑5‑TR states that at least 5 of the following 9 criteria must be met:
- 1. Frantic efforts to avoid real or imagined abandonment
- 2. Unstable and intense relationships (idealizing–devaluing)
- 3. Identity disturbance (unstable self-image or sense of self)
- 4. Impulsivity in at least two self‑damaging areas
- 5. Recurrent suicidal/self‑harm behavior, gestures, or threats
- 6. Affective instability (reactive moods)
- 7. Chronic feelings of emptiness
- 8. Inappropriate, intense anger or inability to control it
- 9. Transient stress-related paranoid ideation or severe dissociation
Let’s break down each of the borderline personality disorder symptoms, with examples and life implications.
Frantic efforts to avoid abandonment
Description: This involves extreme reactions; even over imagined abandonment. These may manifest as:
- Pleading, clinging, calling/texting multiple times a day
- Manipulative behaviors like self-harm threats to stop someone from leaving
Example & life impact: Maria broke up with her partner. Overwhelmed, she threatened to harm herself if he didn’t stay. While this prompted immediate crisis intervention, the relationship remained unstable. Her attempts to avoid abandonment often pushed partners away, reinforcing her fears.
Daily life impact: Leads to relationship exhaustion, social isolation, and frequent crisis encounters.
Unstable and intense relationships
Description: Patterns go from idealization to devaluation (“splitting”).
Example & life impact: Tom idolizes his therapist, then abruptly angrily rejects them when he feels misunderstood. This pattern strains therapy, work, and friendships, creating a whirlwind of attachments and rejections.
Daily life impact: Interpersonal instability, frequent social conflict, difficulty maintaining trust.
Identity disturbance
Description: Marked, persistent unstable self-image or sense of self.
Example & life impact: Lina shifts career paths, hobbies, beliefs swiftly: one day deeply religious, the next atheist. Her sense of self is so fractured it impairs long-term planning and emotional stability.
Daily life impact: Leads to helplessness, dissociation, and unstable professional/academic development.
Impulsivity in at least two areas
Description: Impulsivity in harmful domains like spending, sex, substance use, reckless behavior.
Example & life impact: After emotional stress, Jonas binge-shops expensive items and drives recklessly. Financial chaos ensues; trust from creditors and loved ones shrinks.
Daily life impact: Chronic instability in finance, health, relationships; often accompanied by guilt and shame.
Recurrent suicidal/self-harm behavior
Description: Includes threats, gestures, self-harm, or suicidal actions.
Example & life impact: Emma cuts herself when feeling emotionally overwhelmed. Her family constantly monitors her, house is filled with trauma residue, and she frequently visits emergency services.
Daily life impact: Constant life threat, hospital visits, disrupted trust, decreased autonomy.
Affective instability
Description: Marked mood reactivity (dysphoria, irritability, anxiety) usually lasting hours, rarely days.
Example & life impact: Within hours, Markus switches from elation to despair. He quits his job impulsively and redeems himself days later with the same energy; his environment remains volatile.
Daily life impact: Challenges in work/relationships; unpredictability seen as unreliable or dramatic.
Chronic feelings of emptiness
Description: Persistent boredom, void, lack of meaning.
Example & life impact: Elaine feels nothing even in loving moments. To fill the void, she seeks risky stimuli (sexual, substance-driven) leading to unsafe encounters and intensified internal pain.
Daily life impact: Leads to identity confusion, poor self-care, dysfunctional coping strategies.
Intense anger or inability to control it
Description: Frequent temper, sarcasm, physical fights.
Example & life impact: When criticized, David reacts with fury: breaking objects, yelling at loved ones. He later apologizes profusely, but the damage is done: others avoid interacting with him.
Daily life impact: Creates fractured personal relationships and social isolation.
Transient stress-related paranoid ideation or dissociation
Description: Brief paranoia or dissociative episodes under stress.
Example & life impact: Anna feels someone’s out to harm her. She disconnects, spacing out during conversations. Although short-lived, these episodes erode her credibility, impair her concentration and trust in reality.
Daily life impact: Creates dangerous situations, interpersonal misunderstandings, and stigmatization.
ICD‑11: Severity + Borderline Personality Disorder Symptoms Pattern Specifier
Main difference: ICD‑11 no longer lists personality disorder types. Instead, it assesses:
- 1. Global severity: personality difficulties rated from mild to severe
- 2. Trait qualifiers: Negative affectivity, Detachment, Disinhibition, Dissociality, Anankastia
- 3. Optional Borderline Pattern specifier: Based on ≥5 of the DSM-5 criteria
Severity ratings
- Mild: Some dysfunction in self/interpersonal
- Moderate: Clear dysfunction, hard to develop stable relationships
- Severe: Significant dysfunction, may include transient psychotic-like experiences
Example: Ana scores moderate severity (global instability but intact reality testing). She qualifies for ICD‑11’s “moderate PD with Borderline Pattern.”
Borderline Personality Disorder Symptoms – Trait domains × BPD features
The Borderline Pattern often aligns with:
- Negative affectivity (emotional lability, anxiety)
- Disinhibition (impulsivity, self-damage)
- Dissociality (anger, entitlement, mistrust)
Less so with Detachment or Anankastia.
Example: Ravi is diagnosed with “severe PD, Negative affectivity + Disinhibition + Dissociality, with Borderline Pattern.”
Trait-focused vs. pure categorization
Pros of ICD‑11:
- Clinically useful, simpler diagnostic structure
- Integrates severity and trait features
- Better for treatment planning (targeting emotions, instability, impulsivity)
Cons:
- Adds complexity (requires assessing severity and multiple traits)
- Borderline Pattern specifier debated as redundant, but retained for utility
Borderline Personality Disorder Symptoms – Comparative Summary: DSM‑5‑TR vs. ICD‑11 BPD
Diagnostic structure
Core criteria
Severity assessment
Trait qualifiers
Emphasis on trait profile
Utility for clinical care
Categorical (BPD if ≥5/9 criteria)
Nine specific symptoms
Not explicit
Not included
No
Strong historically
Dimensional (severity + trait + optional Borderline specifier)
Same nine symptoms signal BPD Pattern qualifier ≥5/9
Central: mild, moderate, severe categories
Included (e.g. Negative affectivity, Disinhibition)
Yes: treatment planning via dominant trait domains
Increased focus on transdiagnostic severity and treatment relevance
How Borderline Personality Disorder Symptoms Affect Daily Life
Let’s link each DSM symptom to real-world consequences:
Fear of Abandonment
People with BPD may experience overwhelming anxiety when someone cancels plans, doesn’t reply to a message quickly, or shows signs of emotional distance. This fear can trigger panic, anger, or even self-harming behavior as an attempt to regain attention or prevent perceived abandonment.
It often leads to “testing” loved ones or emotionally clinging to them, which in turn can strain the relationship. In severe cases, even minor separations (like a partner leaving for work) can feel like a devastating rejection.
Unstable and Intense Relationships
Relationships tend to swing between extremes (from idealization to devaluation) which creates confusion, conflict, and emotional exhaustion for both the person with BPD and their loved ones. Arguments may erupt over perceived slights or inconsistent attention.
These intense patterns often result in a cycle of break-ups and reconciliations, or one-sided emotional investments. Trust issues and emotional over-dependence can make it very difficult to maintain long-term healthy connections.
Identity Disturbance
People with BPD often struggle to define who they are, which can lead to frequent changes in career goals, personal values, friendships, and even gender or sexual identity. They may feel like a “chameleon,” adapting to whoever they’re with.
This internal confusion can cause a lack of direction in life, chronic dissatisfaction, and frustration. It often results in starting and quitting jobs or studies repeatedly and feeling empty despite external achievements.
Impulsivity in Potentially Self-Damaging Areas
Many individuals with BPD engage in impulsive behaviors like reckless driving, binge eating, overspending, substance abuse, or unsafe sex (especially when they feel emotionally distressed). These behaviors may bring short-term relief but often lead to long-term consequences.
They may lose jobs, struggle financially, or get into legal trouble due to impulsive decisions. These actions are usually followed by intense shame and regret, which worsen emotional instability.
Recurrent Suicidal Behavior or Self-Harm
Self-injury (e.g., cutting or burning) or suicide threats and attempts are not uncommon in BPD and are often triggered by interpersonal conflict or intense emotional pain. Although not always intended as suicidal acts, these behaviors are serious cries for help.
Such incidents can result in emergency hospital visits, emotional trauma for family members, and increased social isolation. Over time, they can severely impact one’s ability to work or maintain stable relationships.
Affective Instability (Rapid Mood Swings)
Mood shifts in BPD can be dramatic and rapid: from intense happiness to despair, anger, or fear, often within hours. These changes are typically reactive to interpersonal stressors or perceived rejection.
Such instability can cause misunderstandings in the workplace or in social settings, where others may see the person as unpredictable or volatile. As a result, friendships may dwindle and professional opportunities may be lost.
Chronic Feelings of Emptiness
Many individuals with BPD describe feeling empty, hollow, or like they don’t exist (especially when they are alone or not receiving emotional validation). This void can be so painful that people try to fill it with distractions or risky behavior.
Over time, this emotional emptiness may contribute to substance abuse, binge behaviors, or codependent relationships. It also reduces motivation for long-term goals, often leading to feelings of purposelessness or depression.
Inappropriate, Intense Anger
Anger in BPD can escalate quickly and often feels uncontrollable. It may be triggered by seemingly small events, such as a partner not answering the phone or a coworker making a critical remark.
Explosive reactions can alienate friends, family, and colleagues, leading to isolation. In extreme cases, this can result in physical confrontations, job loss, or legal consequences such as restraining orders or arrests.
Paranoia or Dissociation Under Stress
Under high stress, individuals with BPD may experience paranoid thoughts (e.g., believing others are plotting against them) or dissociative episodes where they feel detached from their body, thoughts, or surroundings.
This can impair decision-making, memory, and attention, making it hard to function in school, work, or family life. Important meetings may be missed, or they may feel unable to participate in key life events because they feel unreal or emotionally frozen.