What is Borderline personality disorder?
Borderline Personality Disorder (BPD) is a complex and often misunderstood mental health condition characterized by intense emotional instability, impulsive behaviors, a distorted self-image, and chronic fears of abandonment. Individuals with BPD often struggle to regulate their emotions and may find it difficult to maintain stable relationships. These challenges can lead to a recurring pattern of intense mood swings, emotional outbursts, and unstable interpersonal connections.
Key Facts About BPD
- BPD affects an estimated 1.6% to 5.9% of the general population.
- It is more commonly diagnosed in women, though recent research suggests that it may be equally prevalent in men, but underdiagnosed.
- BPD often develops in early adulthood and may be linked to early life trauma, such as neglect, abuse, or unstable caregiving environments.
- Many individuals with BPD also suffer from co-occurring disorders, including depression, PTSD, anxiety disorders, eating disorders, or substance use disorders.
Want to know which 3 treatments are effective for BPD?
People with BPD typically go to great lengths to avoid real or imagined abandonment. This fear of rejection can result in behaviors that are emotionally intense or even self-destructive, such as starting arguments, threatening self-harm, or making frantic efforts to prevent someone from leaving. Ironically, these behaviors often push others away, reinforcing the person’s deep fear of being alone. This pattern can become a painful and self-perpetuating cycle.
Common symptoms of BPD include intense and unstable interpersonal relationships, a shifting sense of identity, impulsive or reckless behavior, emotional instability, chronic feelings of emptiness, and inappropriate or poorly controlled anger. Individuals may also experience temporary, stress-related paranoia or dissociative symptoms. These symptoms can lead to significant distress and impairment in daily functioning.
Side-note: the risks of ChatGPT!
People with BPD often experience intense emotional swings, unstable relationships, and a strong fear of abandonment. When such individuals turn to ChatGPT for emotional support, the bot’s unconditional affirmations and lack of boundaries may unintentionally mimic the idealization phase in their relationships—only to be followed by frustration when the AI fails to meet complex emotional needs. This dynamic can trigger emotional dysregulation, reinforce black-and-white thinking, and deepen feelings of invalidation or rejection. Instead of providing stable emotional grounding, ChatGPT’s simulated empathy may amplify the emotional volatility that characterizes BPD. For more information, please read our informative article on the risks of chatGPT on mental health.
Borderline Personality Disorder Symptoms explained
Is There Hope for People With BPD?
Yes, absolutely. Although BPD can be deeply disruptive, effective treatments are available. Dialectical Behavior Therapy (DBT) and Schema Therapy are two evidence-based approaches that have shown strong results in helping individuals with BPD lead more stable and fulfilling lives. With the right therapeutic support, many people see significant improvement in how they handle emotions, build relationships, and view themselves.
Jump to:
- BPD symptoms explained
- What causes BPD?
- How is borderline diagnosed?
- BPD treatment.
- BPD self-test.
- Coping with BPD.
- Interesting BPD facts.
- Living with someone who has BPD.
- Online counseling for BPD.
- Take me to the homepage.
At Barends Psychology Practice, we offer (online) therapy for borderline personality disorder. Contact us to schedule a first, free of charge, online session.
What Are the Symptoms and Traits of Borderline Personality Disorder?
Borderline Personality Disorder (BPD) is one of the most common and most thoroughly researched personality disorders [1]. It significantly impacts how a person perceives themselves, relates to others, and handles emotional experiences. Symptoms often begin in adolescence or early adulthood and are frequently associated with traumatic or invalidating early life experiences.
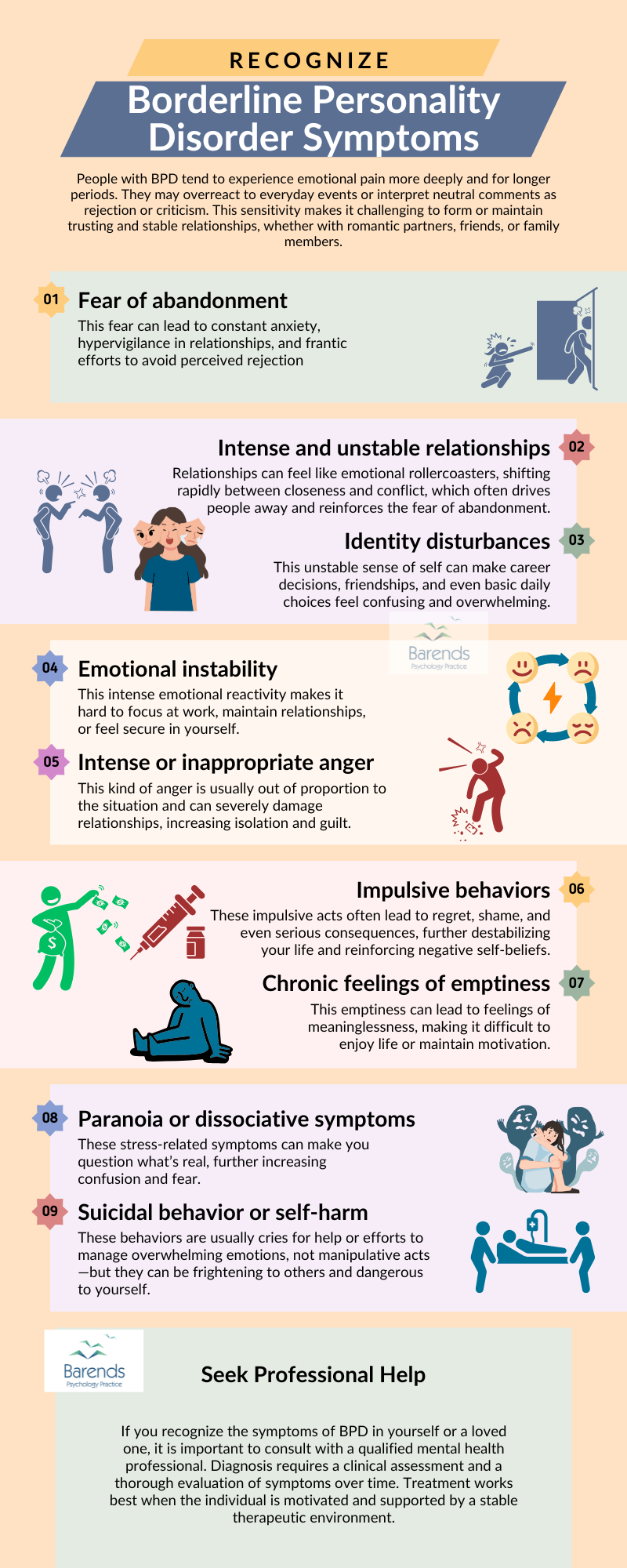
People with BPD tend to experience emotional pain more deeply and for longer periods. They may overreact to everyday events or interpret neutral comments as rejection or criticism. This sensitivity makes it challenging to form or maintain trusting and stable relationships, whether with romantic partners, friends, or family members.
Core symptoms include:
- An intense fear of abandonment, whether real or imagined.
Example: You panic when your partner doesn’t reply to your message within an hour. You might send multiple follow-ups, accuse them of ignoring you, or suddenly withdraw to “punish” them. This fear can lead to constant anxiety, hypervigilance in relationships, and frantic efforts to avoid perceived rejection—even when no rejection is happening. - Intense and unstable relationships.
Example: You might idealize a new friend or partner, believing they are perfect. But if they disappoint you in any way—like forgetting a plan—you may suddenly see them as cruel or untrustworthy. Relationships can feel like emotional rollercoasters, shifting rapidly between closeness and conflict, which often drives people away and reinforces the fear of abandonment. - Identity disturbances
Example: One day you feel like you know exactly who you are and what you want—perhaps you decide to become a teacher. A few days later, you abandon that plan entirely, feeling lost or like a fraud. This unstable sense of self can make career decisions, friendships, and even basic daily choices feel confusing and overwhelming. - Impulsive behaviors
Example: You go on a shopping spree with money you don’t have, binge eat, drive recklessly, or have unprotected sex with strangers—all to escape emotional pain. These impulsive acts often lead to regret, shame, and even serious consequences, further destabilizing your life and reinforcing negative self-beliefs. - Intense or inappropriate anger
Example: You explode in rage when your friend arrives ten minutes late, yelling or saying hurtful things you later regret. This kind of anger is usually out of proportion to the situation and can severely damage relationships, increasing isolation and guilt. - Paranoia or dissociative symptoms under stress.
Example: After a conflict at work, you feel like your coworkers are plotting against you or talking behind your back. Or you may feel “numb” or disconnected from your body for hours. These stress-related symptoms can make you question what’s real, further increasing confusion and fear. - Chronic feelings of emptiness, as if nothing brings joy or meaning.
Example: Feeling numb and disconnected even during activities or moments that used to be pleasurable, like spending time with friends. - Suicidal behavior or self-harm
Example: After a breakup or argument, you may cut yourself, overdose, or send messages suggesting that others would be better off without you. These behaviors are usually cries for help or efforts to manage overwhelming emotions, not manipulative acts—but they can be frightening to others and dangerous to yourself.
(Advertisement. For more information, please continue reading.)
How These Symptoms Create Chaos in Daily Life
The core symptoms of BPD often overlap and feed into one another, creating a vicious cycle that disrupts nearly every area of daily life:
- Work becomes unpredictable, as emotional instability and impulsivity can affect concentration, relationships with colleagues, and the ability to manage responsibilities.
- Relationships are often unstable and emotionally intense, leading to frequent conflicts, breakups, or social isolation.
- Self-esteem fluctuates rapidly, leaving you feeling unsure of who you are or what you’re capable of.
- Daily routines can be hard to maintain because mood swings and impulsive decisions interfere with consistency and planning.
Life with BPD can feel like you’re constantly reacting to emotional emergencies, making long-term goals and stability feel out of reach. But with proper treatment and support, these patterns can be broken, and life can become more predictable, secure, and fulfilling.
Treatment Options for BPD
Although BPD can feel overwhelming, effective treatment is available. At Barends Psychology Practice, we emphasize that individuals with BPD can absolutely recover and lead fulfilling lives. Two of the most evidence-based treatment modalities are Dialectical Behavior Therapy (DBT) and Schema Therapy. DBT helps individuals develop skills for emotion regulation, distress tolerance, mindfulness, and interpersonal effectiveness. Schema Therapy focuses on uncovering and healing maladaptive schemas that stem from unmet emotional needs in early life.
Therapy for BPD is usually long-term and requires a strong therapeutic alliance, but research consistently shows that symptoms can significantly improve with consistent treatment. Many individuals report enhanced emotional control, better relationships, and an improved sense of self after several months of therapy.
Living with BPD: Challenges and Coping
Living with BPD often means grappling with intense emotional reactions and difficulty maintaining balance in life. This emotional dysregulation can lead to impulsive actions, such as substance abuse, binge eating, or reckless spending, which may temporarily relieve pain but often increase distress in the long run. People with BPD may also experience deep shame and guilt following these episodes, creating a vicious cycle.
At Barends Psychology Practice, we help clients identify their emotional triggers and replace self-destructive coping strategies with healthier alternatives. Emotion regulation, self-compassion, and developing a stable sense of identity are all critical goals in the healing process.
Family members and loved ones of someone with BPD may feel overwhelmed, confused, or emotionally drained. Psychoeducation, couples therapy, or family counseling can be extremely helpful in improving communication and reducing misunderstandings. Understanding that the behaviors are symptoms—not intentional cruelty—is key to supporting someone with BPD.
When to Seek Professional Help
If you recognize the symptoms of BPD in yourself or a loved one, it is important to consult with a qualified mental health professional. Diagnosis requires a clinical assessment and a thorough evaluation of symptoms over time. Treatment works best when the individual is motivated and supported by a stable therapeutic environment.
At Barends Psychology Practice, we offer both in-person and online therapy for Borderline Personality Disorder. Your first session is free of charge and without obligation. We are here to help you take the first steps toward a more stable and meaningful life.
Literature used for this article
-
- [1] Grant, B. F., et al., 2009. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: results from the wave 2 national epidemiologic survey on alcohol and related conditions. J Clin Psychiatry, 69, 533-545.
(Advertisement. For more information, continue reading.)