Coping with borderline personality disorder
Borderline personality disorder (BPD) is a difficult personality disorder to deal with. Coping with borderline personality disorder requires persistence, patience, rest, a healthy rhythm, and a good friend or therapist to reach out to. Without these key ingredients coping with borderline personality disorder can be extremely difficult and damaging (think of relationships and self-harm).
This page focuses on coping skills for those people with BPD who rather try things themselves before considering reaching out to a professional. Depending on the severity of BPD, these self help tips are effective if you follow the instructions. However, professional counseling is highly recommended, because treatment is effective and helps you deal with crisis situations as well.
NOTE: in case you have suicidal thoughts or want to self-harm, I strongly recommend you to reach out to a professional!!
Want to know which 3 treatments are effective for BPD?
Jump to:
- What is borderline personality disorder?
- BPD symptoms explained
- What causes Borderline personality disorder?
- How is borderline diagnosed?
- Borderline personality disorder treatment.
- Borderline personality disorder self-test.
- Living with someone who has BPD.
- Interesting borderline personality disorder facts.
- Online counseling for Borderline personality disorder.
- Take me to the homepage.
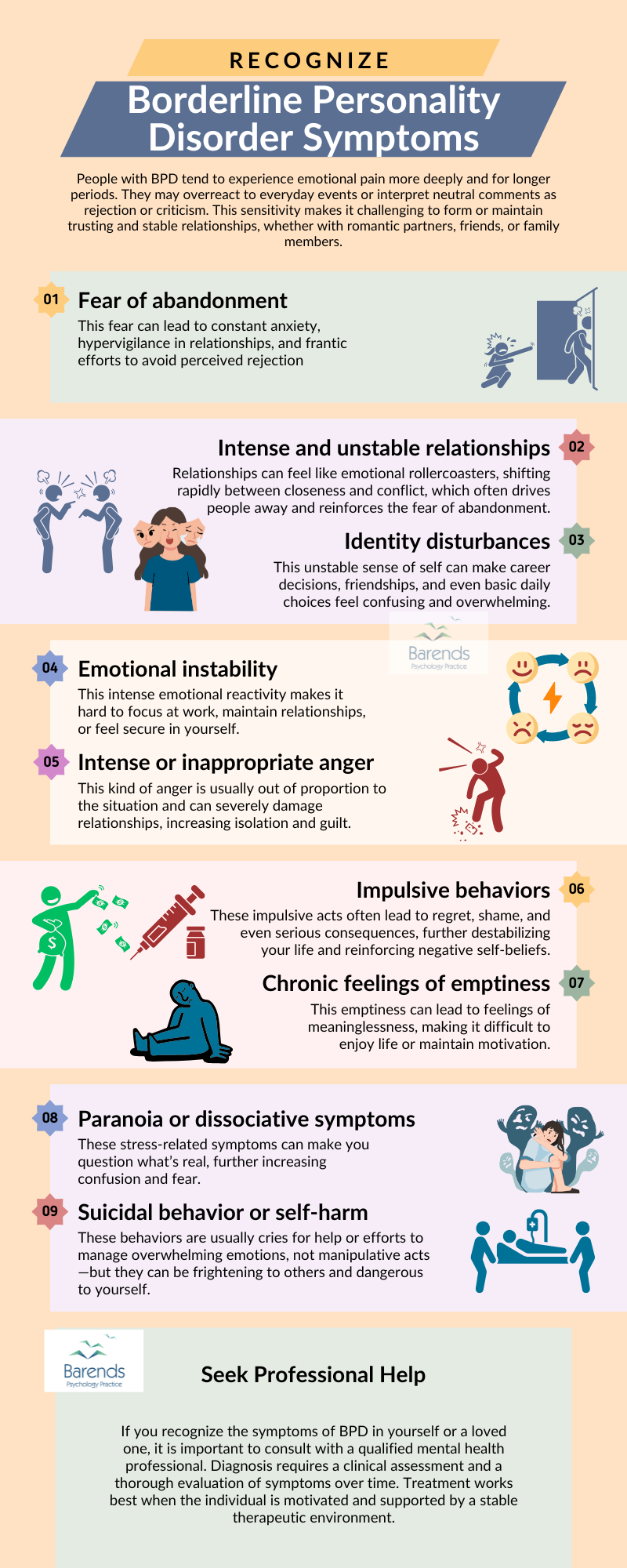
Borderline Personality Disorder – Easy and quick explanation of the BPD symptoms and the differences between DSM-5-TR and ICD-11!
At Barends Psychology Practice, we offer (online) therapy for borderline personality disorder. Contact us to schedule you first, free of charge, online session today.
Reducing self-harm behaviour:
- People with BPD often use self-harm as a way to regulate their emotions, express pain, or punish themselves. Damaging one’s body produces physical pain, which can temporarily reduce emotional pain—such as sadness, guilt, rage, emptiness, or self-loathing. In the short term, self-harm may seem to relieve emotional suffering, but in the long run, the emotional pain inevitably returns, often leading to repeated self-harming. Unfortunately, self-harm is by no means a real solution: it leaves scars, causes physical pain, can be very dangerous, and may lead to feelings of guilt or shame afterward. Most people who self-harm try to hide it from those close to them because of this shame, which further isolates them and exacerbates BPD symptoms.
- Approximately 75% of people with BPD attempt suicide, and 10% die by suicide (usually before the age of 40) [1], [2]. Co-occurring substance abuse or major depressive disorder significantly increases both the frequency and severity of suicide attempts [1]. A history of childhood sexual abuse is also associated with a higher number of suicide attempts [3]. People often attempt suicide because they genuinely want to die. While some professionals believe suicide attempts may be a cry for attention, this view has been disputed by others.
- 1. Confide in someone: Opening up about your secret can be both frightening and relieving. Try to find someone you trust completely—perhaps a friend, teacher, or relative. Talk to them (or write, call, etc.) about the feelings and situations that lead you to self-harm, but try to avoid describing the self-harming in detail. Let them know if you’re looking for a listening ear or advice. Keep in mind that the person you confide in may react with shock, concern, fear, or even anger. These are normal reactions, even if they’re difficult to accept. Give the person time to process what you’ve shared. Don’t be discouraged if their initial reaction is not what you hoped for. Ultimately, reaching out to others is an important step in coping with borderline personality disorder. Isolation and BPD are a harmful combination.
- 2. Identify your self-harm triggers: What feelings or situations lead you to self-harm? Write down specific examples—it will make it easier to find healthier alternatives. Initially, try to avoid those triggers while developing better coping strategies. For example, if losing a debate makes you feel worthless, try to avoid arguments for now and learn more about discussion techniques. If drug use makes you more vulnerable to self-harm, then try to avoid drugs altogether.
Some people struggle to identify what they’re feeling. They fear their emotions will overwhelm them or won’t go away. But feelings typically last only about 10 minutes before they begin to fade. Try to allow yourself to experience your emotions; with time, it gets easier.
- 3. Find new coping mechanisms: Stopping self-harm without a replacement strategy is unlikely to succeed. Try these steps in order:
- (a) Reduce the damage caused by self-harming (e.g. cutting less deeply);
- (b) Replace self-harming with healthier alternatives (e.g. writing on your skin with a red marker or snapping an elastic band on your wrist);
- (c) Direct your urges toward objects instead of yourself (e.g. crushing ice cubes, hitting pillows or cushions);
- (d) Distract yourself (e.g. spend time with others, play video games, listen to music, or exercise).
Distraction helps you tolerate overwhelming feelings, which reduces the urge to self-harm.
- 4. Reach out to a professional: A professional counsellor specialized in Dialectical Behaviour Therapy (DBT) can significantly reduce the number of suicide attempts and self-harm behaviours [4]. A therapist can also help you identify the deeper issues behind your triggers. Many people with BPD have experienced significant trauma, which may underlie their self-harming behaviour. Unfortunately, it can be very difficult to make these connections on your own.
- [1] Black, D. W., Blum, N., Pfohl, B., & Hale, N., 2004. Suicidal behaviour in borderline personality disorder: prevalence, risk factors, prediction, and prevention. Journal of Personality Disorders, 18, 226-239.
- [2] Paris, J., and Zweig-Frank, H., 2001. A 27-year follow-up of patients with borderline personality disorder. Comprehensive Psychiatry, 42, 482-487.
- [3] Soloff, P. H., Lynch, K. G., & Kelly, T. M., 2002. Childhood abuse as a risk factor for suicidal behaviour in borderline personality disorder. Journal of Personality Disorders, 16, 201-214.
- [4] Giesen-Bloo, J., van Dyck, R., Spinhoven, P., van Tilburg, W., Dirksen, C., van Asselt, T., Kremers, I., Nadort, M., & Arntz, A., 2006. Outpatient psychotherapy for borderline personality disorder randomized trial of schema-focused therapy vs transference-focused psychotherapy. Arch Gen Psychiatry, 63, 649-658.
What can someone do to reduce self-harm behaviour?
(Advertisement. For more information, please scroll down.)
PLEASE NOTE: If you feel that these steps may not work for you, it is especially important to reach out to a professional. And even if they do help, consider seeking professional support anyway. These steps may reduce self-harming behaviour, but they do not address the unresolved trauma that continues to be triggered in the present. Coping with borderline personality disorder is a long and often difficult journey. Professional guidance can help you navigate this process and promote real healing.
Coping with borderline personality disorder – coping skills.
Here are some practical coping tips to help reduce the impact of BPD symptoms. These strategies are not a substitute for therapy, so always consider working with a professional trained in treating BPD.
Side-note: the risks of ChatGPT!
People with BPD often experience intense emotional swings, unstable relationships, and a strong fear of abandonment. When such individuals turn to ChatGPT for emotional support, the bot’s unconditional affirmations and lack of boundaries may unintentionally mimic the idealization phase in their relationships—only to be followed by frustration when the AI fails to meet complex emotional needs. This dynamic can trigger emotional dysregulation, reinforce black-and-white thinking, and deepen feelings of invalidation or rejection. Instead of providing stable emotional grounding, ChatGPT’s simulated empathy may amplify the emotional volatility that characterizes BPD. For more information, please read our informative article on the risks of chatGPT on mental health.
Coping with BPD, part 1: the first 4 coping skills
1. Track Your Emotions
People with BPD often struggle to recognize their own emotions and understand where they come from. Take a moment several times a day to ask yourself: “How have I been feeling these past two hours?” Pay attention to any tension in your body; it may be linked to unprocessed emotions. Follow up by asking: “Why have I been feeling this way?” Be specific. For example: instead of “I’m angry because of my stupid boyfriend,” say, “I’m angry because he forgot to pick me up again.” The more precise you are, the easier it is to manage your emotions.
If you start noticing patterns, it is likely caused by specific triggers. These triggers may come from unprocessed traumatic events from the past. It may be worth exploring these with your therapist.
2. Avoid Impulsive Decisions
Don’t respond immediately to emotionally charged situations. If someone asks you something or upsets you, take a moment to pause. Repeat the question, ask for clarification, or reflect before answering. Wait at least a week before making life-changing decisions, and talk them over with people you trust. This delay reduces impulsive actions and improves communication.
3. Practice Mindfulness
Mindfulness can help you stay grounded in the present moment and reduce emotional overwhelm. Practice observing your thoughts and feelings without judgment. Try breathing exercises or body scans to center yourself during distressing moments. Self-soothing activities (such as listening to calming music, going for a walk, or holding something comforting) can also be part of your mindfulness toolkit.
4. Challenge Negative Thoughts
When you experience intense emotions, ask yourself: “What triggered this?” Try to identify which thoughts came first and which emotions are tied to them. For example, if your partner doesn’t pick up the phone, you might think, “They’re ignoring me” (leading to sadness), or “Maybe they’re with someone else” (triggering fear or anger). Writing down your thoughts and separating facts from assumptions can help calm you down and provide clarity.
(Advertisement. For more tips, please scroll down.)
5. Set Realistic Goals
Coping with BPD requires persistence and patience. Set small, achievable goals and celebrate progress, no matter how minor it seems. Building habits gradually is more effective and sustainable than making big changes all at once.
6. Increase Tolerance of Uncertainty
People with BPD often feel overwhelmed by uncertainty, which leads to anxiety and catastrophic thinking. Practice writing down multiple explanations for ambiguous situations (e.g., why someone didn’t answer your call) and rate them by likelihood. Identify your worst fear and treat it as a hypothesis, then test it logically or in therapy. Most fears are unrealistic, and learning this can reduce panic and emotional distress. Always consult a professional before doing exposure exercises on your own.
7. Build Support Carefully
Not all relationships are emotionally safe. If certain people make you feel sad, angry, or anxious, consider limiting contact with them, especially before important events like meetings or date nights. Surround yourself with people who support your healing, and talk about emotional triggers with your therapist so you can work through them safely.
8. Stick to a Healthy Rhythm
Sleep and eat at consistent times. When your body lacks routine, you’re more likely to feel tired, irritable, and emotionally reactive. Having a regular rhythm helps regulate mood and reduces the chances of emotional outbursts. A stable schedule gives your body and brain time to mentally prepare and stay balanced.
9. Use Crisis Plans
Have a plan ready for when you feel emotionally overwhelmed. This can include emergency contacts, calming activities, distraction techniques, or written reminders of coping strategies. Keeping your plan accessible gives you something to lean on when you feel like losing control.
(Advertisement. For more tips, please scroll down.)
10. Use Positive Self-Talk
What you say to yourself matters. Remind yourself of your worth and of the people who care about you. Ask your partner or close friends to list things they appreciate about you and read these during tough moments. Just like elite athletes use self-talk to perform better, you can use it to improve emotional stability and self-esteem.
Final Note
Coping with BPD is not a part-time task — it’s a full-time commitment that requires courage, patience, and ongoing effort. Be kind to yourself as you try these strategies, and reach out for professional support when needed. You don’t have to do it alone.
Literature used for this article