PTSD treatment
Post-traumatic stress disorder (PTSD) treatment can help you regain control over your life. Psychotherapy is the primary treatment, sometimes complemented by medication. PTSD treatment can significantly reduce or completely eliminate symptoms. In many cases, especially when EMDR therapy is applied, only a few sessions are needed.
However, treatment duration may be longer for individuals who have experienced multiple, prolonged, or repetitive traumatic events. Other factors influencing treatment length include PTSD severity, co-occurring mental health disorders, and the complexity of trauma processing.
Medication is recommended in cases of severe trauma where the individual dissociates during psychotherapy. Dissociation occurs when a person mentally disconnects from their immediate surroundings. In severe cases, a PTSD patient may dissociate to the extent that the therapist or others cannot “reach” them. This is a defense mechanism to protect against emotional and physical pain.
At Barends Psychology Practice, we offer online Eye Movement Desensitization and Reprocessing (EMDR) and exposure therapy to treat PTSD, as both are highly effective and cost-efficient [1]. Below is an overview of different PTSD treatments and their effectiveness.
At Barends Psychology Practice, we treat Post-traumatic stress disorder Online and in person. Book your first, free session now. Contact us.
Jump-to:
Eye movement desensitization and reprocessing (EMDR)
According to Francine Shapiro, PTSD may occur when a traumatic event overwhelms normal cognitive and neurological coping mechanisms. This can lead to an inadequate way of storing and processing the memory, isolating it from the brain’s normal networks. The goal of EMDR is to reprocess these distressing memories, reducing their emotional impact and enabling the development of healthier coping mechanisms.
Effectiveness of EMDR:EMDR is as effective as Cognitive Behavioral Therapy (CBT) [1],[2],[3] but often requires fewer sessions. A key advantage of EMDR is that patients do not need to share details of their trauma if they find it too painful or humiliating. Even without discussing specifics, EMDR can still be highly effective.
How Does EMDR Treatment Work?
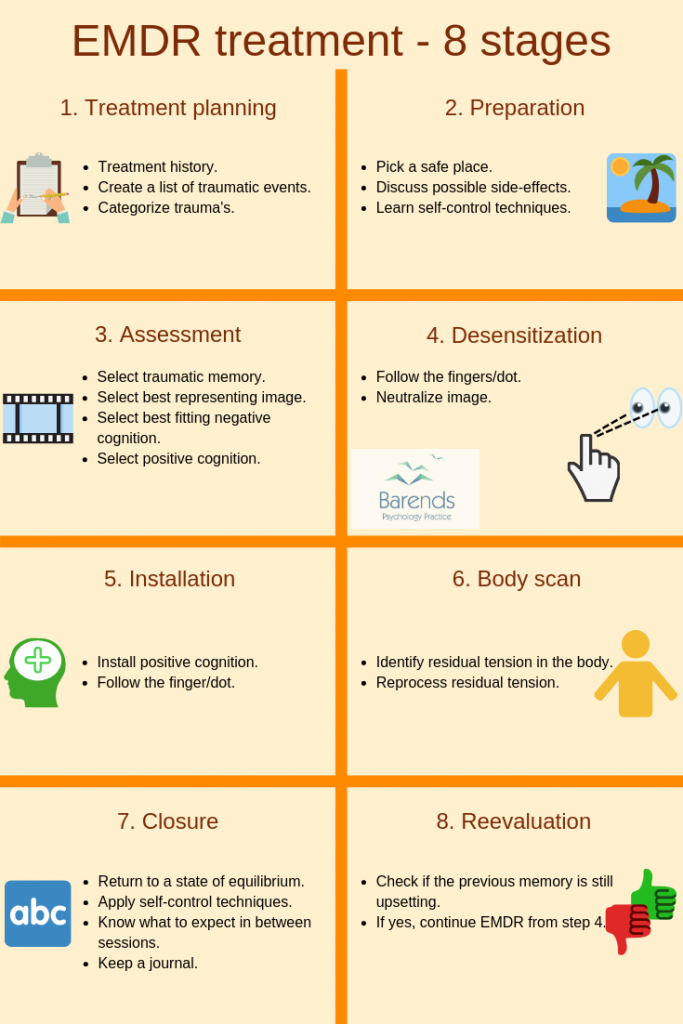
EMDR consists of eight stages, all crucial to PTSD treatment. While originally developed for in-person therapy, EMDR can also be conducted online, provided it is supervised by a trained EMDR therapist.
We have provided a traumatic events form for you to fill out before your first EMDR session. If you have any questions, feel free to contact us.
Stage 1 – Treatment Planning
For EMDR to be most effective, it is important to select the most representative image of a traumatic event. In cases of multiple traumatic experiences, treatment typically starts with the most distressing, earliest, or most significant event. If a client prefers not to discuss details of the trauma, they can assign a name to the event and the selected image. The therapist may ask neutral questions, such as: “Do you see yourself in the image?”
Stage 2 – Preparation
The therapist prepares the client for EMDR by explaining the process, ensuring a sense of safety, and introducing relaxation techniques.Stage 3 – Assessment
Selecting the correct image for processing is crucial. Choosing the wrong image may reduce EMDR’s effectiveness. Some traumatic events involve multiple images, which must be prioritized for treatment.
The Subjective Units of Disturbance Scale (SUDS) is used to rate distress levels from 0 (neutral) to 10 (most distressing). The therapist also identifies negative beliefs associated with the trauma and helps establish positive alternative thoughts.
Stage 4 – Desensitization
The therapist guides the patient through bilateral stimulation (e.g., eye movements, tapping, or sounds) to reduce emotional distress.
Stage 5 – Installation
Once the distress level (SUDS) reaches 0 or 1, the positive cognition is reinforced. This is measured using the Validity of Cognition (VoC) scale from 1 (not true at all) to 7 (completely true).
Stage 6 – Body Scan
A body scan helps identify residual physical tension related to the trauma. This step enhances EMDR’s effectiveness by addressing lingering physical symptoms.
Stage 7 – Closure
The therapist and client discuss the session’s experiences, potential side effects, and the importance of keeping a journal to track emotional changes.
Stage 8 – Reevaluation
At the start of the next session, the therapist checks whether the processed image still triggers distress. If it does, desensitization continues. If not, the image is considered neutralized—unless new trauma occurs.
Cognitive Behavioral Therapy (CBT)
CBT aims to change negative thought patterns that contribute to PTSD symptoms. By challenging irrational fears and replacing distressing thoughts, CBT helps reduce PTSD-related stress.
CBT for PTSD typically involves exposure therapy and cognitive restructuring. Cognitive restructuring focuses on identifying and challenging unhelpful beliefs related to the trauma, such as self-blame or feelings of helplessness. Through these techniques, CBT empowers individuals to process their trauma more adaptively, reducing distress and improving daily functioning.Effectiveness of CBT CBT is a effectiveness of CBT as PTSD treatment: CBT is a safe and effective treatment for both chronic and acute PTSD. It is also the most widely used PTSD treatment in the USA.
(Advertisement. For more information, please scroll down.)
Exposure therapy
Exposure therapy is a key component of CBT for PTSD, designed to help individuals gradually confront trauma-related memories, emotions, and situations they have been avoiding. This is done in a safe and controlled manner, reducing the power these triggers hold over them. There are different types of exposure, including imaginal exposure (revisiting the traumatic event in one’s mind and describing it in detail) and in vivo exposure (directly facing real-life situations that are reminders of the trauma but are not actually dangerous). For example, a survivor of a car accident who avoids driving may gradually start sitting in a parked car, then riding as a passenger, and eventually driving short distances, with the guidance of a therapist. Through repeated exposure, the brain learns that these triggers are not inherently dangerous, reducing fear and avoidance over time. Effectiveness of Exposure Therapy Exposure therapy is highly effective Exposure treatment is an effective for both acute and chronic PTSD.
Medication for PTSD
Medication is usually prescribed alongside therapy because it does not eliminate PTSD-related flashbacks or distressing emotions. Antidepressants – SSRIs Selective Serotonin Reuptake Inhibitors (SSRIs) are the most common PTSD medications. They can help reduce anxiety, depression, and panic symptoms, but they take 6 to 8 weeks to show effects. However, SSRIs are not always effective:- Only 2 out of 4 clinical studies found SSRIs to be more effective than a placebo (a fake treatment).
- Patients often need to try multiple SSRIs before finding one that works. For more information on SSRIs, see our Treating Depression section.
PTSD treatment – literature
[1] Rothbaum, B. O., Astin, M. C., & Marsteller, F. (2005). Prolonged exposure versus eye movement desensitization and reprocessing (EMDR) for PTSD rape victims. Journal of Traumatic Stress: Official Publication of The International Society for Traumatic Stress Studies, 18, 607-616.
[2] Lee, C., Gavriel, H., Drummond, P., Richards, J., & Greenwald, R. (2002). Treatment of PTSD: Stress inoculation training with prolonged exposure compared to EMDR. Journal of clinical psychology, 58, 1071-1089.
[3] Seidler, G. H., & Wagner, F. E. (2006). Comparing the efficacy of EMDR and trauma-focused cognitive-behavioral therapy in the treatment of PTSD: a meta-analytic study. Psychological medicine, 36, 1515-1522.